Recurrent ankylotic mass treated with aggressive resection and myofascial flap with aggressive physiotherapy

*Corresponding author: Alka Mariam Mathew, Post Graduate Student, Department of OMFS, Ragas Dental College and Hospital, 2/102, SH 49, Uthandi, Tamil Nadu - 600 119, India. alkamathew08@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mathew AM, Vijayaranghan S, Baburaj D, Veerabahu M, Sankar D. Recurrent ankylotic mass treated with aggressive resection and myofascial flap with aggressive physiotherapy. J Global Oral Health 2020;3(1):36-40.
Abstract
We are presenting a case with multiple recurring ankylosis, as the child had exhibited the clinical signs and symptoms of an ankylotic right temporomandibular joint. She was operated for the 1st time when she was 6 years old with poor compliance and was reoperated with a distraction unit when she was 10 years old. The research points out to frequent relapses in younger patients operated as they had less compliance relative to the adult ankylotic patients. Henceforth, we dealt with an aggressive approach of planning only on the resection of the mass and if the mouth opening ensues to progress with further correction of the asymmetry and the residual defect. The patient had nil mouth opening and hence was consented for tracheostomy, and fiber-optic intubation was arranged. The aggressive resection of the ankylotic mass was done and the cavity was lined with temporalis myofascial flap. This was followed by aggressive physiotherapy. The patient now has 28 mm of mouth opening and is continuing aggressive physiotherapy for the same. After 6 months of surgery, the patient is planned to undergo corrective jaw surgery for the asymmetry present.
Keywords
Recurrent ankylosis
Myofascial flap
Contralateral coronoidectomy
Aggressive physiotherapy
Fiber- optic intubation
INTRODUCTION
Temporomandibular joint (TMJ) ankylosis is a disorder, wherein a stiff joint leads to restriction of mouth opening. It is due to a fibrous or a bony union between the head of the condyle of the mandible and the glenoid fossa of temporal bone. It may be caused by direct or indirect trauma to the condyle, infection, degenerative joint disease, prolonged mandibulomaxillary fixation, as a sequel to a surgical reduction of the condyle, inflammatory conditions such as rheumatoid arthritis, systemic diseases such as ankylosing spondylitis and scleroderma, and polyarthritis and last but not the least benign and malignant conditions within the joint and outside the joint.
It is classified into true or false ankylosis by Kazanjian. In true ankylosis, there is bony or fibrous adhesion between surfaces of joint within joint capsule, whereas Sawhney describes both intra- articular and extra-articular ankylosis, wherein the latter, the pathology lies in the surrounding structures. It is one of the most overlooked and undermanaged conditions in the initial management of trauma and results in disability and subsequent morbidity.
It is a serious and disabling condition that may cause a problem in facial growth, impairment of mastication, deglutition, digestion, speech, facial asymmetry, and in severe cases as bird facies, poor oral hygiene with rampant caries. In case of bilateral ankylosis, the patients present with growth disturbances in the mandible and its corresponding maxilla giving rise to the bird facies with nil mouth opening and airway compromise. These presenting features bring about low social self-esteem to the patient with aggravating psychological stress that they personally start seeking treatment in their early adulthood if not treated until then.
Severity of ankylosis is diagnosed by evaluating the degree to which mouth opening is restricted. X-rays, CT scans, or MRI tests determine the abnormality in the bony or soft tissue formations in the joint. The treatment of TMJ ankylosis poses a significant challenge because of technical difficulties and high incidence of recurrence. Team approach is required for resolving functional, esthetic (cosmetic), psychological (emotional), or social problems associated with ankylosis. Report of an adult female is presented here whose treatment was carried out in a stage-wise protocol.
This paper describes our experience with the efficacy of interpositional arthroplasty with temporalis myofascial flap.
CASE PRESENTATION
An 18-year-old female patient presented with a chief complaint of nil mouth opening [Figure 1] since birth. She presented with gross facial deformity (bird facies), convex profile, retrognathic chin, micrognathia, double chin, decrease thyromental distance, decrease hyomental distance, and reduced lower facial height. On palpation no movement was elicited on the right joint and the left exhibited mild rotational movement only. She was diagnosed with the right bony temporomandibular joint ankylosis and left fibrous ankylosis of the TMJ. She gave a history of ankylosis release by gap arthroplasty in 2006 and placement of a distraction device in 2010 after which she developed reankylosis. Investigations taken include OPG and CT [Figure 2] to visualize the joint, assess the airway and for STL model printing [Figure 3]. CT revealed a bony ankylosis with respect to the right TMJ and well-defined glenoid fossa on the left side showing fibrous ankylosis, thereby eliminating the need for a surgical option for the left joint.

- Pre-operative restricted mouth opening.
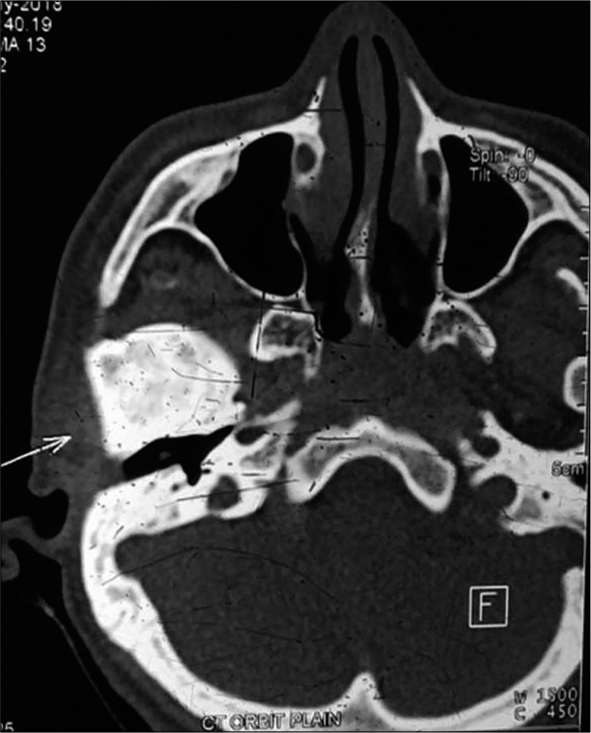
- Pre-operative CT showing the ankylotic mass.
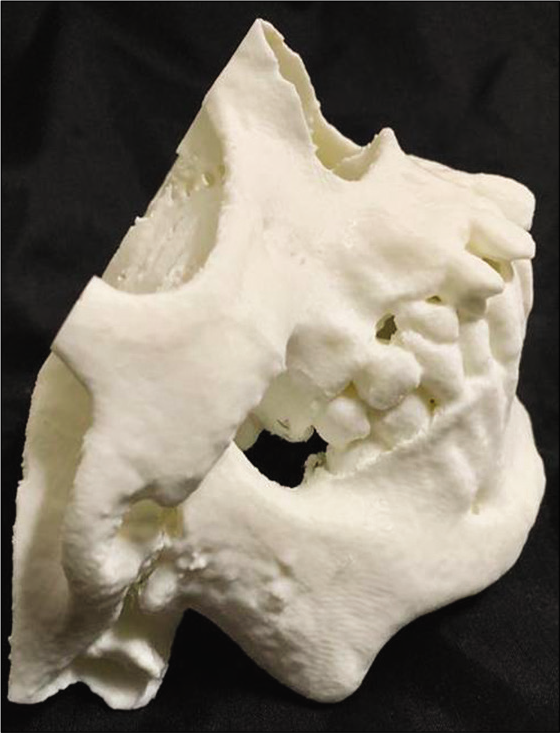
- Pre-operative stereolithographic model.
Considering the difficulty with the airway and the compliance of the patient, a meticulous planning was considered to release the ankylosis with interpositional arthroplasty using a temporalis myofascial flap and contralateral coronoidectomy was decided. With the difficult airway, the patient had a history of two failed attempts of blind intubation elsewhere; hence, the surgery was canceled twice. The patient was consented for tracheostomy if the fiber-optic intubation failed. The patient was prepared for GA and underwent fiber- optic nasotracheal intubation with no untoward events and tracheostomy was deferred.[1]
Blind intubation was described by W. Magill and E. S. Rowbotham, in 1921. The blind nasal intubation is done in awake patient. A well-lubricated nasotracheal tube is gently passed through the most patent nostril. The bevel of the tube should be pointing laterally so as to avoid trauma to concha. During the insertion of the nasotracheal tube, the patient’s head is extended, and the tracheal cartilage is pressed down gently. The tube is advanced while listening to the breath sounds and the advancement of tube is stopped before the bifurcation of trachea. The insertion of the nasotracheal tube is confirmed by bilateral lung auscultation and capnography.[2]
Fiber-optic intubation was first described by Peter Murphy, in 1967. It is a technique where a flexible endoscope with a tracheal tube loaded along its length is passed through the glottis. The tracheal tube is then pushed off the endoscope and inserted into the trachea, and the endoscope is withdrawn. The patient is awake during the entire procedure and is advised to breathe oronasally and to swallow continuously.
An inverted hockey stick incision with temporal extension was used. On reaching the temporoparietal fascial layer, the superficial temporal artery and vein were identified.[3] Above the zygomatic arch, the superficial layer of the temporal fascia was incised in an oblique line running from the tragus to the superior temporal line. This incision was parallel to the inverted hockey stick incision. A mosquito hemostat was used to dissect bluntly along the external auditory canal in an anterior-medial direction to the level of the temporomandibular joint capsule. While elevating this “pocket,” we used a blade to extend the fascial release to the most inferior part of the tragus. This technique allowed us to retract the superficial temporal vessels anteriorly and preserve this vital pedicle of our temporal fascial flap [Figure 4].[4] Approximately 1 cm of bony mass causing ankylosis was removed using piezo [Figures 5 and 6]. A trial mouth opening brought about a 20 mm and henceforth the contralateral coronoidectomy was decided to be performed. The contralateral coronoid process was exposed through intra-oral approach followed by stripping temporalis attachment. Coronoid was held with Kocher’s forcep and the osteotomy cut was made extending from the depth of sigmoid notch to the anterior border of ramus. After the osteotomy was completed, the coronoid was removed. Closure was done with 3.0 Vicryl.
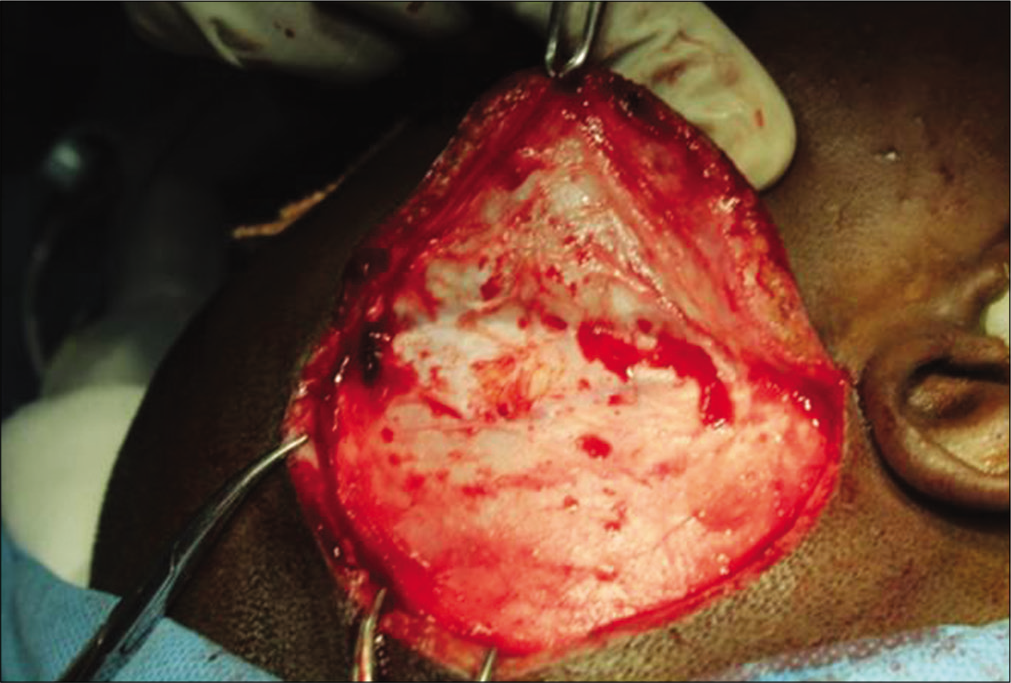
- Temporalis myofascial flap elevation.
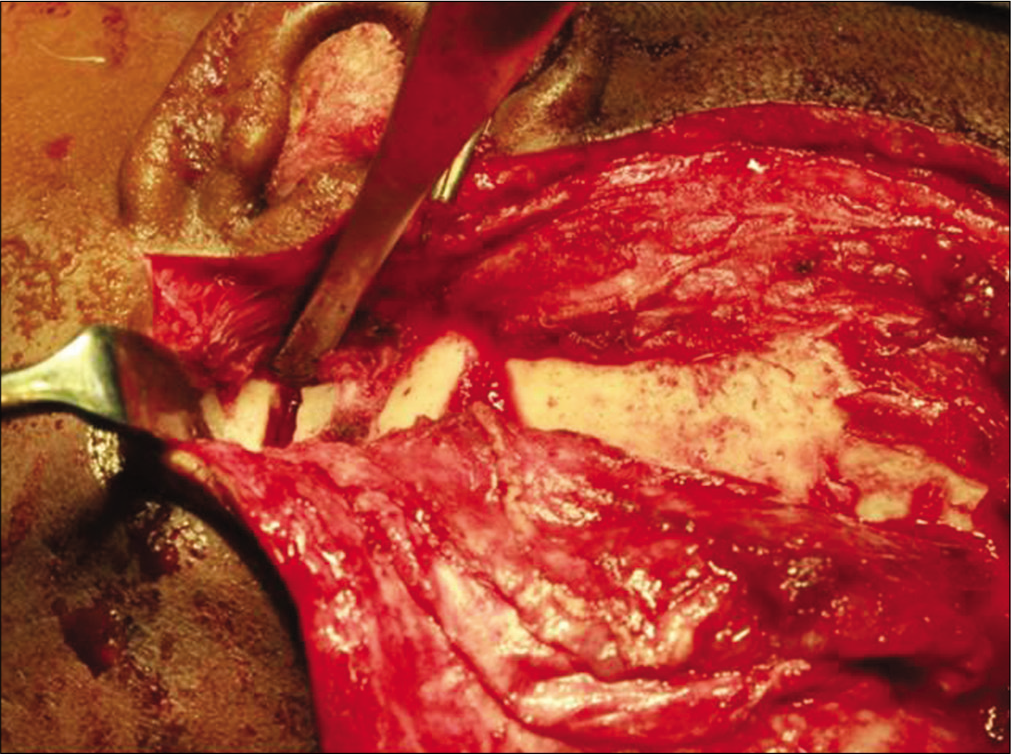
- Removal of ankylotic mass through osteotomy cuts.

- Excised ankylotic mass.
Further the Interpositional arthroplasty was done using the pedicled Temporalis myofascial flap by tunnelling through the zygomatic arch [Figure 7]. Haemostasis was secured and a drain was placed. The wound was closed layer by layer using with 3.0 Vicryl and 4.0 Ethilon after noting intraoperative passive mouth opening.

- Temporalis myofascial flap as an interpositional flap that is lining the cavity.
The patient was given appropriate antibiotics and analgesics as required. The patient’s mouth opening was monitored postoperatively which was 25 mm, 28 mm and 30 mm in the 3rd, 4th, and 5th post-operative days, respectively. Post- operative mouth opening exercises were initiated on the 3rd postoperative day and later, both active and passive exercises were allowed. Pre- and post-operative mouth opening were measured by inter-incisor distance and compared. The patient was followed up at 1 and 3 months. In the 2-month interval, the mouth opening was maintained at 30 mm [Figures 8 and 9].

- Increased postoperative mouth opening.

- Post-operative OPG of the patient.
DISCUSSION
TMJ ankylosis earlier in 1938 was classified into two types by Kazanjian[5] as intra-articular and extra-articular ankylosis. The present classification includes bony, fibrous, fibro- osseous, complete, and incomplete.[6,7] Congenital ankylosis was described by Burbet, in 1936; however, there were controversies to the fact that ankylosis is not a congenital deformity due to trauma at birth. The causes and treatment of TMJ ankylosis have been well documented[8] with trauma and infection identified as the two leading causes.[9] Trauma has been cited as the most common underlying reason responsible for ankylosis; however, systemic disorders (e.g., rheumatoid arthritis) and local infections (e.g., otitis media) also can cause bilateral or unilateral TMJ ankylosis.[10] By improving the immediate management protocol of condylar fracture and proper application of antibiotics to address ear infections, the prevalence of ankylosis has been decreased significantly in recent years. In children, TMJ ankylosis can result in mandibular retrognathism with associated esthetic and functional deficits. Therefore, treatment should be initiated as soon as the condition is recognized, with the main objective of reestablishing joint function and harmonious jaw function.[11]
The pathogenesis of the TMJ ankylosis is described in a sequence of events. The intra-articular vascular supply at the traumatized joint is increased which develops fibrosis and ultimately results in excessive localized bone formation.[12] This excessive bone mass has the potential of continual growth and does not have a neoplastic nature,[13] but the presence of abnormal bony mass restricts mandibular movement, which may subsequently lead to loss of the functional matrix of bone and muscle interaction and consequently result in growth failure.[14]
Maximum mouth opening in the presence or absence of pain is a clinical indicator of traumatized condyle.[15] In addition to routine extraoral and intraoral photographs, Towne’s projection, posteroanterior, and cone-beam CT (3D) radiographs, stereolithographic model is commonly used for this purpose.
In our case, we have followed the Kaban protocol[12] by aggressive resection of the ankylotic mass of 1.5 cm which contains both the affected condyle and coronoid process of the ipsilateral side, this was followed by contralateral coronoidectomy and the joint cavity was lined with temporalis myofascial flap and the patient is now on aggressive physiotherapy and cooperative for post-operative jaw exercise which helps in the prevention of reankylosis.
Topazian reported a recurrence rate of 53% in gap arthroplasty without interposition.[16] The zone of excision should be sufficiently wide to prevent ankylosis but should produce little change in the vertical height of mandible.
Interpositional arthroplasty addresses the main drawbacks of the gap arthroplasty method. In this technique, surgeons try to fill the gap with autogenous graft materials including skin, dermis, flap of temporalis muscle, cartilage, or even alloplastic materials like Silastic.[15]
Temporalis myofascial flap is a locally available axial pattern flap which is based on the deep temporal arteries. This vascularized flap has fewer chances of subsequent resorption and fibrosis. The advantages of the temporalis myofascial flap are reliable blood supply, ease of elevation, and proximity to temporomandibular joint and incision is hidden in the hairline. The result of our case was in favor of temporal myofascial flap as an interposition material which aids in the prevention of reankylosis.[16]
In the literature, there are two main reasons for reankylosis after surgical release including inadequate resection of the ankylotic mass intraoperatively and also the absence of patient compliance regarding post-operative jaw exercise.[11]
CONCLUSION
The main aim of the treatment of temporomandibular joint ankylosis is not only to achieve adequate mouth opening but also to prevent recurrence of ankylosis. Interpositional arthroplasty using vascularized temporalis fascia flap is a very reliable method to prevent recurrence of ankylosis and it also avoids the disadvantages of alloplastic materials as well as non-vascularized autogenous tissues.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Blind nasal intubation as an alternative to difficult intubation approaches. J Dent Anesth Pain Med. 2015;15:181-4.
- [CrossRef] [PubMed] [Google Scholar]
- Airway regional anesthesia for awake fiberoptic intubation. Reg Anesth Pain Med. 2002;27:180-92.
- [CrossRef] [Google Scholar]
- Interposition arthroplasty in post-traumatic temporomandibular joint ankylosis: A retrospective study. Indian J Plast Surg. 2009;42:182-7.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical anatomy and blood supply of the fascial layers of the temporal region. Plast Reconstr Surg. 1986;77:17-28.
- [CrossRef] [Google Scholar]
- Ankylosis of temporomandibular joint. Surg Gynaecol Obstet. 1938;67:333-48.
- [CrossRef] [Google Scholar]
- Bony ankylosis of the temporomandibular joint: Follow-up of 70 patients treated with arthroplasty and acrylic spacer interposition. Plast Reconstr Surg. 1986;77:29-40.
- [CrossRef] [PubMed] [Google Scholar]
- Temporomandibular joint ankylosis: Review of the literature and report of two cases of bilateral involvement. J Oral Surg. 1975;33:792-803.
- [Google Scholar]
- Ankylosis of the temporo-mandibular joint. Plast Reconstr Surg (1946). 1948;3:464-77.
- [CrossRef] [PubMed] [Google Scholar]
- Temporomandibular joint ankylosis. J Indian Acad Oral Med Radiol. 2016;28:334-6.
- [CrossRef] [Google Scholar]
- Comprehensive management of temporomandibular joint ankylosis-state of the art. In: A Textbook of Advanced Oral and Maxillofacial Surgery. Vol 2. London: Intech Openn; 2014.
- [CrossRef] [Google Scholar]
- A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 1990;48:1145-51.
- [CrossRef] [Google Scholar]
- New perspectives in the management of cranio-mandibular ankylosis. Int J Oral Maxillofac Surg. 2000;29:337-40.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical investigation of early post-traumatic temporomandibular joint ankylosis and the role of repositioning discs in treatment. Int J Oral Maxillofac Surg. 2006;35:1096-101.
- [CrossRef] [PubMed] [Google Scholar]
- Full-thickness skin graft interposition after temporomandibular joint ankylosis surgery. A study of 31 cases. Int J Oral Maxillofac Surg. 1999;28:330-4.
- [CrossRef] [PubMed] [Google Scholar]
- The role of temporal fascia interposition in the surgical treatment of TMJ ankylosis. Annals. 2004;10:265-7.
- [Google Scholar]






