Translate this page into:
Assessment of oral health-related quality of life among head-and-neck cancer patients attending cancer care center at Kanchipuram, Tamil Nadu – A cross-sectional study

*Corresponding author: Sekar Aswini, Postgraduate Student, Department of Public Health Dentistry, Vivekanandha Dental College for Women, Namakkal, Tamil Nadu, India. dent.aswinisekar@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Aswini S, Shavi GR, Shankar S, Sanga R, Lalithambigai G, Rahila C, et al. Assessment of oral health-related quality of life among head-and-neck cancer patients attending cancer care center at Kanchipuram, Tamil Nadu – A cross-sectional study. J Global Oral Health 2021;4(1):20-6.
Abstract
Objectives:
Oral health is closely related to general health and people’s quality of life (QoL), through affecting their oral functions and social interactions. This study aims to assess the oral health-related QoL among head-and-neck cancer (HNC) patients attending cancer care center at Kanchipuram, Tamil Nadu.
Materials and Methods:
A cross-sectional questionnaire-based study was conducted among 340 HNC patients between August and October 2019 attending Government Arignar Anna Memorial Cancer Hospital and Research Institute in Kanchipuram District of Tamil Nadu. The questionnaire has two parts. The 1st part consists of demographic characteristics and cancer-related details. The 2nd part was the European Organization of Research and Treatment of Cancer QoL in HNC patients (EORTC QLQ H&N-35) questionnaire.
Results:
Among 340 patients, 72.4% were male and 27.6% were female. The majority of them had Stage II cancer. The main factors affecting oral health related QoL (OHRQoL) were taking painkillers, loss of sexual interest, difficulty in social contact, teeth problems, loss of taste, and smell senses. Significant association found between pain (P = 0.000), sense (P = 0.003), speech (P = 0.000), social eating (P = 0.016), social contact (P = 0.005), teeth problems (P = 0.031), dry mouth (P = 0.000), sticky saliva (P = 0.000), cough (0.002), feeling ill (P = 0.003), nutritional supplement (P = 0.042), and lost weight (P = 0.034) with respect to various treatment modalities. Based on the OHRQoL scores, those who were treated surgically alone had better QoL than others.
Conclusion:
We found that surgically treated HNC patients had better OHRQoL than others. Thus, Oral-Health related Quality of Life assessment can be used to analyse the outcome of treatment, patient satisfaction and their sense of self. We need to build a broader care protocol which satisfies/improves the demands arising from the patients.
Keywords
Oral health-related quality of life
EORTC QLQ H&N-35
Head and neck
INTRODUCTION
The head-and-neck cancers (HNCs) are a heterogeneous collection of malignancies that arise from the lips, oral cavity, tongue, nose, tonsil, larynx, nasopharynx, oropharynx, hypopharynx, paranasal sinus, parotids, and thyroid.[1] Worldwide, the HNC accounts for more than 650,000 cases and 330,000 deaths annually. Overall, 57.5% of global HNC occur in Asia, especially in India. HNC in India accounted for 30% of all cancers.[2,3]
Patients with HNC have multiple, unique, and challenging symptoms due to their disease and treatment such as xerostomia, taste disturbances, dietary restrictions, dysphagia, pain, fatigue, distortions of physical appearance, infirmity, weight loss, and permanent disfigurement,. which has a severe impact on the patients quality of life (QoL).[4] Treatment usually consists of surgery, radiotherapy, chemotherapy, or combination. Treatment strategies are, therefore, not only directed at increasing the chances of cure but also at diminishing the impact of treatment on QoL.[5]
Quality of Life is a multidimensional concept which looks at how patients feel about themselves in the context of a medical condition.[6] The subjective evaluation of oral health-related QoL “reflects people’s comfort when eating, sleeping, and engaging in social interaction; their self-esteem; and their satisfaction concerning their oral health.”[7] An individual’s health-related QoL will be affected if the oral health is worsened. No study has been conducted on HNC patients regarding their oral health related QoL (OHRQoL) in South India. Quantifying subjective experience of OHRQoL has been a challenging issue. Hence, a questionnaire-based study was conducted to assess OHRQoL in HNC patients attending cancer care center in Kanchipuram, Tamil Nadu.
MATERIALS AND METHODS
The present study is a cross-sectional study conducted at Government Arignar Anna Memorial Cancer Hospital and Research Institute in Kanchipuram District of Tamil Nadu. The study was conducted from August to October 2019. The study protocol was discussed and permission was obtained from the Directorate of Medical Education, Government of Tamil Nadu. Ethical clearance was then obtained from the Government Arignar Anna Memorial Cancer Hospital and Research Institute’s ethical committee. Written consent was also obtained from the patients.
Inclusion and exclusion criteria
Patients diagnosed with HNC aged 18 years and above of both sexes receiving treatment and willing to participate in the study were recruited. Patients with imprecise and incomplete information on clinical and histological data, having cancers other than head and neck, mentally challenged, and speech impaired are excluded from the study. Subjects were selected by purposive sampling technique. The sample size was calculated with the formula n=4pq/l2 with the prevalence of HNC in India 30%.
Data collection procedure
The questionnaire used in the study consists of two parts. The 1st part consists of demographic characteristics and cancer-related details which include the site of cancer, duration of illness, stage of cancer, and type of treatment. The 2nd part was the European Organization of Research and Treatment of Cancer QoL in HNC patients (EORTC QLQ H&N-35) questionnaire.
The EORTC QLQ questionnaire was (1) cancer specific, (2) multidimensional in structure, (3) appropriate for self-administration (i.e., brief and easy to complete), and (4) applicable across a range of cultural settings. The module EORTC QLQ H&N-35 incorporates seven multi-item scales/ domains that assess pain, swallowing, senses (taste and smell), speech, social eating, social contact, and sexuality experienced during the past week. There are also 11 single items. The personal information and QLQ questionnaire were completed by the patient and disease characteristics were extracted from the patient’s hospital records. In the case where the patient is illiterate, the questions are read by the investigator without guiding them to give a specific answer. The questionnaire was translated into the local language (Tamil). The reliability of the tool was established by administering the QLQ questionnaire to 20 patients with HNC and Cronbach’s alpha was calculated as 0.92.
Scoring criteria
Out of 35 questions/items, 30 questions are scored on 4-point Likert scale (“not at all – 1,” “a little – 2,” “quite a bit – 3,” and “very much – 4”) and 5 questions have yes/no type (2, 1) response format.
The scores are linear transformed into 0–100 scales with the formula S=(RawScore-1/Range)×100.
A high score for a symptom scale/item scale score represents a higher response level of symptomatology/problems. After obtaining the scores, they were entered into a Microsoft Excel spreadsheet, and a master table was prepared. The data were analyzed using the software Statistical Package for the Social Sciences version 16, Inc., Chicago, IL, USA, with the level of significance kept at P < 0.05. Both descriptive and inferential statistics were computed. The descriptive data are presented as frequencies and mean values. ANOVA test was done to assess the association of OHRQoL with site, stage, and treatment modalities of HNC.
RESULTS
[Table 1] shows the demographic variables, habits, and disease-related details of the patients. About 72.4% were male; 50.9% were aged between 41 and 60 years; 36.2% were illiterates; 45% were elementary workers; the majority of them had tobacco habit; buccal mucosa and tongue are the most common site of HNC. The majority of them stopped their tobacco habit after diagnosis (88.5%). We divided the site of cancer into six categories for ease of analysis.
| Variable | n(%) |
|---|---|
| Gender | |
| Male | 246 (72.4) |
| Female | 94 (27.6) |
| Age (in years) | |
| 20–40 | 67 (19.7) |
| 41–60 | 173 (50.9) |
| 61–80 | 100 (29.4) |
| Level of education | |
| Illiterate | 123 (36.2) |
| Primary school | 102 (30.0) |
| Middle school | 76 (22.4) |
| High school | 27 (7.9) |
| Diploma/intermediate | 6 (1.8) |
| Graduate | 6 (1.8) |
| Occupation | |
| Unemployed | 31 (9.1) |
| Elementary occupation | 153 (45.0) |
| Plant, machine operators, and assemblers | 15 (4.4) |
| Craft and related trade workers | 24 (7.1) |
| Skilled agricultural and fishery workers | 50 (14.7) |
| Shop and market sales workers | 49 (14.4) |
| Clerks | 3 (0.9) |
| Technicians and associate professionals | 15 (4.4) |
| Marital status | |
| Married | 326 (95.9) |
| Unmarried | 5 (1.5) |
| Widowed | 6 (1.8) |
| Divorced | 3 (0.9) |
| Socioeconomic status | |
| Lower | 66 (19.4) |
| Upper lower | 212 (62.5) |
| Lower middle | 56 (16.3) |
| Upper middle | 6 (1.8) |
| Tobacco habit | |
| Smoking | 114 (33.5) |
| Smokeless | 104 (30.6) |
| Combined | 113 (33.2) |
| No habit | 9 (2.6) |
| Stopped tobacco habit after diagnosis | |
| Yes | 301 (88.5) |
| No | 30 (8.8) |
| No habit | 9 (2.6 |
| Site of cancer | |
| Buccal mucosa | 69 (20.3) |
| Tongue | 65 (19.1) |
| Lips | 14 (4.1) |
| Floor of the mouth | 6 (1.8) |
| Palate | 6 (1.8) |
| Alveolus | 9 (2.6) |
| Maxilla | 6 (1.8) |
| Mandible | 9 (2.6) |
| Oropharynx | 47 (13.8) |
| Nasopharynx | 8 (2.4) |
| Hypopharynx | 36 (10.6) |
| Larynx | 43 (12.6) |
| Others | 22 (6.5) |
| Staging of cancer | |
| Stage I | 21 (6.2) |
| Stage II | 144 (42.4) |
| Stage III | 125 (36.8) |
| Stage IV | 50 (14.7) |
| Duration of illness (months) | |
| <6 | 189 (55.6) |
| 6–12 | 124 (36.5) |
| >12 | 27 (7.9) |
| Treatment modalities | |
| Only radiotherapy | 81 (23.8) |
| Only surgery | 60 (17.6) |
| Surgery + radiotherapy | 52 (15.3) |
| Radiotherapy + chemotherapy | 75 (22.1) |
| Surgery + radiotherapy + chemotherapy | 57 (16.8) |
| Not yet started | 15 (4.4) |
| Visiting the dentist | |
| Every 1–5 years | 14 (4.1) |
| Emergency only | 243 (71.5) |
| Never | 83 (24.4) |
Buccal mucosa, tongue, lips, the floor of the mouth, palate, alveolus, maxilla, and mandible were clubbed into a single category, that is, oral cavity. The remaining categories were oropharynx, nasopharynx, hypopharynx, larynx, and others. The “others” category includes malignancies of the thyroid and salivary glands.
[Graph 1] shows the percentage of all the domains and single items of the OHRQoL H&N-35 questionnaire. Based on the scores calculated, the major factors affecting OHRQoL were taking painkillers, loss of sexuality, teeth problems, feeling ill, weight loss, and social contact. The domains and single items of the QoL questionnaire were compared according to sites of the tumor, stage of cancer, and type of treatment method.
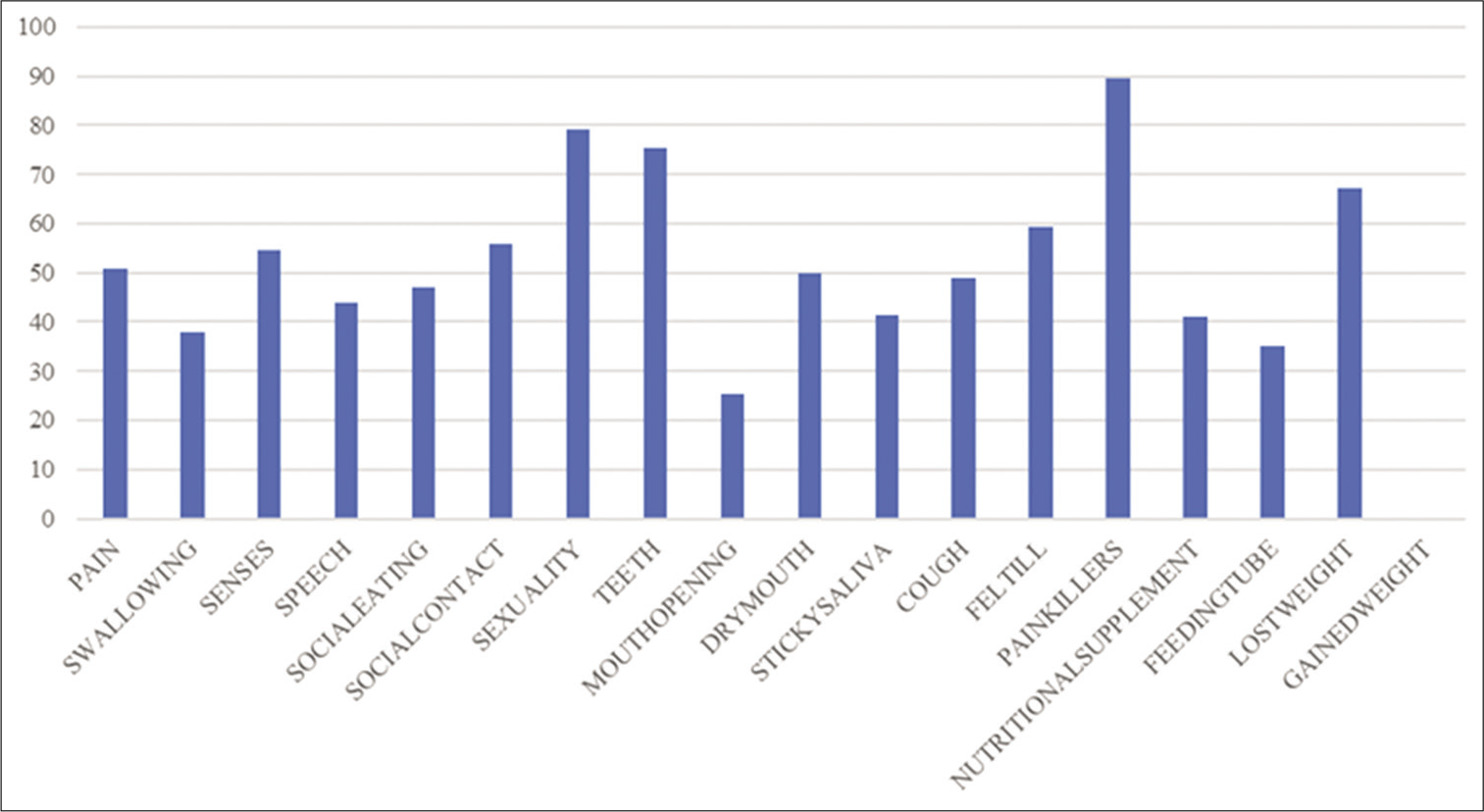
- Percentage distribution of factors affecting OHRQoL.
[Table 2] shows a comparison of OHRQoL items with the stage of cancer. Stage IV HNC with high scores illustrates that OHRQoL is impaired severely in comparison with other stages of the disease. After carrying out ANOVA, statistically significant differences were found for pain, swallowing, sense, speech, social eating, social contact, dry mouth, sticky saliva, falling ill, and nutritional supplement.
| EORTCH&N35 | Mean | P-value | |||
|---|---|---|---|---|---|
| Stage I | Stage II | Stage III | Stage IV | ||
| Pain | 26.19 | 41.31 | 57.39 | 70.03 | 0.000* |
| Swallowing | 29.36 | 33.86 | 37.43 | 47.43 | 0.009* |
| Sense | 53.96 | 50.11 | 55.55 | 64.74 | 0.044* |
| Speech | 36.41 | 39.13 | 45.95 | 56.0 | 0.003* |
| Social eating | 40.47 | 42.08 | 49.73 | 56.08 | 0.011* |
| Social contact | 42.53 | 49.78 | 59.84 | 68.26 | 0.000* |
| Sexuality | 74.60 | 80.14 | 76.45 | 84.61 | 0.180 |
| Teeth | 73.01 | 73.75 | 74.07 | 83.33 | 0.081 |
| Reduced mouth opening | 26.98 | 24.82 | 26.19 | 23.71 | 0.942 |
| Dry mouth | 52.38 | 40.42 | 54.49 | 64.10 | 0.000* |
| Sticky saliva | 38.09 | 34.75 | 43.65 | 55.12 | 0.001* |
| Cough | 42.85 | 49.64 | 49.73 | 48.07 | 0.858 |
| Felt ill | 47.61 | 56.97 | 59.52 | 69.87 | 0.005* |
| Painkiller | 85.71 | 85.81 | 93.65 | 92.30 | 0.160 |
| Nutritional supplement | 28.57 | 35.46 | 42.06 | 59.61 | 0.014* |
| Feeding tube | 23.80 | 33.33 | 34.12 | 46.15 | 0.241 |
| Lost weight | 71.42 | 66.66 | 64.28 | 75.0 | 0.553 |
*Denotes P value <0.05 and statistically significant.
[Table 3] shows a comparison of OHRQoL domains/items with the site of cancer. Nasopharynx and oropharynx cancer patients have crumbled OHRQoL than other HNC. Statistically significant differences were found for swallowing, sense, social eating, sexuality, teeth, reduced mouth opening, sticky saliva, cough, and falling ill.
| EORTCH&N35 | Mean | P-value | |||||
|---|---|---|---|---|---|---|---|
| Oral cavity | Oropharynx | Nasopharynx | Hypopharynx | Larynx | Others | ||
| Pain | 51.17 | 52.12 | 59.37 | 47.22 | 47.92 | 53.03 | 0.669 |
| Swallowing | 35.58 | 43.97 | 56.25 | 40.97 | 31.63 | 31.81 | 0.044* |
| Sense | 59.45 | 56.73 | 83.33 | 40.74 | 42.17 | 50.75 | 0.000* |
| Speech | 42.04 | 44.91 | 53.41 | 53.18 | 47.62 | 32.53 | 0.124 |
| Social eating | 51.87 | 46.27 | 41.66 | 43.75 | 34.18 | 44.31 | 0.009* |
| Social contact | 58.22 | 53.04 | 66.66 | 50.37 | 48.97 | 63.63 | 0.131 |
| Sexuality | 84.26 | 76.59 | 87.50 | 66.66 | 76.19 | 66.66 | 0.000* |
| Teeth | 76.59 | 79.43 | 83.33 | 83.33 | 58.50 | 77.27 | 0.000* |
| Reduced mouth opening | 31.27 | 21.27 | 29.16 | 14.81 | 16.32 | 21.21 | 0.002* |
| Dry mouth | 50.37 | 49.64 | 66.66 | 42.59 | 46.25 | 62.12 | 0.176 |
| Sticky saliva | 43.07 | 46.09 | 54.16 | 22.22 | 40.13 | 46.96 | 0.004* |
| Cough | 44.56 | 56.02 | 58.33 | 69.44 | 42.17 | 48.48 | 0.002* |
| Felt ill | 61.04 | 56.73 | 79.16 | 63.88 | 48.29 | 60.60 | 0.013* |
| Painkiller | 88.20 | 93.61 | 100.0 | 97.22 | 83.67 | 90.90 | 0.280 |
| Nutritional supplement | 41.01 | 57.44 | 50.00 | 38.88 | 28.57 | 36.36 | 0.113 |
| Feeding tube | 38.20 | 25.53 | 50.00 | 25.00 | 42.85 | 22.72 | 0.168 |
| Lost weight | 64.60 | 74.46 | 100.00 | 80.55 | 57.14 | 63.63 | 0.053 |
*Denotes P value <0.05 and statistically significant.
[Table 4] shows the comparison of OHRQoL factors with various treatment modalities given for HNC. Patients who were treated surgically had better OHRQoL than other combined treatment modalities. Factors such as pain, sense, speech, social eating, social contact, teeth, dry mouth, sticky saliva, cough, felt ill, nutritional supplement, and weight loss were found to be statistically significant.
| EORTCH&N35 | Mean | P-value | |||||
|---|---|---|---|---|---|---|---|
| RT alone | Surgery alone | RT+ Chemo | Surgery + RT | Surgery + RT + Chemo | Not yet started | ||
| Pain | 41.36 | 42.89 | 54.13 | 57.67 | 63.33 | 49.40 | 0.000* |
| Swallowing | 34.55 | 32.92 | 34.61 | 39.80 | 45.45 | 29.16 | 0.076 |
| Sense | 50.00 | 49.72 | 50.96 | 55.48 | 70.60 | 48.80 | 0.003* |
| Speech | 34.91 | 38.90 | 38.36 | 54.37 | 55.06 | 42.38 | 0.000* |
| Social eating | 44.81 | 39.89 | 42.62 | 51.42 | 57.12 | 42.26 | 0.016* |
| Social contact | 47.56 | 53.00 | 59.10 | 56.14 | 64.66 | 69.52 | 0.005* |
| Sexuality | 76.82 | 75.40 | 80.12 | 76.31 | 87.87 | 85.71 | 0.053* |
| Teeth | 76.42 | 69.39 | 71.15 | 76.31 | 83.63 | 71.42 | 0.031* |
| Reduced mouth opening | 26.42 | 22.40 | 25.64 | 25.00 | 25.45 | 30.95 | 0.935 |
| Dry mouth | 60.56 | 10.92 | 62.82 | 58.77 | 66.06 | 0.00 | 0.000* |
| Sticky saliva | 48.78 | 13.66 | 55.12 | 40.78 | 59.39 | 0.00 | 0.000* |
| Cough | 50.00 | 39.89 | 36.53 | 58.33 | 52.72 | 64.28 | 0.002* |
| Felt ill | 55.69 | 53.55 | 52.56 | 64.03 | 69.69 | 64.28 | 0.003* |
| Painkiller | 84.14 | 88.52 | 92.30 | 94.03 | 87.27 | 100 | 0.203 |
| Nutritional supplement | 32.92 | 36.06 | 48.07 | 42.10 | 56.36 | 21.42 | 0.042* |
| Feeding tube | 25.60 | 40.98 | 38.46 | 35.52 | 40.00 | 28.57 | 0.386 |
| Lost weight | 63.41 | 65.57 | 51.92 | 72.36 | 80.00 | 78.57 | 0.034* |
*Denotes P value <0.05 and statistically significant.
DISCUSSION
QoL is the way with which the individual faces the different aspects of his/her life as a whole. It is associated with the individual’s degree of satisfaction found in family life, love life, social and environmental life, and the very existential sense. To assess the QoL of the patients affected by HNC, it is important to better understand the impact of the disease and its treatment on the patient’s daily routine, and improve the care protocol with more encompassing clinical, social and rehabilitation support measures.[8] de Graeff et al. and Alicikus et al. found that the male:female ratio was 4:1, in the present study, it was 3:1.[9,10]
Meyer et al. found 64% of tobacco users among their studied patients’ groups whereas in our study it was 97.3%.[11,12] Most of the subjects belonged to upper lower and lower socioeconomic status and this complied with the results of Khandekar et al. who reported that the low SES may be a risk factor for poor oral hygiene, and in this way, it further increases the risk for cancer.
In the present study, the common location for the tumor was buccal mucosa and it correlates with the results of Shavi et al.[13]
Factors such as painkillers intake, loss of sexual interest, teeth problems, weight loss, the feeling of being ill, and difficulties in maintaining social contact greatly pull down the OHRQoL in our study and it was found to be analogous with the results of Campbell et al.[14] Social contact helps to cope with stress, whereas here poor social contact hints that they may be embarrassed by their disabilities or health problems such that they tend to isolate themselves to avoid social interaction out of fear that they would be judged or stigmatized. Sometimes, rather than embarrassment, the disability itself and a person’s lack of a support network can be the cause of social isolation.
Fang et al.[15] found that patients presented with the tumor in Stage IV had lower QoL than patients in Stages I, II, and III, and this is consistent with the results of the present study.[15] This proclaims that approaching the physician without neglecting the initial stage of the disease will prevent the spread of the disease to other places, make treatment easier and also the QoL will not be greatly affected.
Dry mouth and sticky saliva are found to be significantly high in patients treated with radiotherapy and chemotherapy. This is due to the damage caused by these treatment modalities on salivary glands. Due to the quantitative and qualitative salivary changes, patients become more prone to dental diseases with important impairment in QoL.[16-18]
Based on the scores, patients treated surgically alone had better OHRQoL than others and it is similar to the findings of Barrios et al.[19] The results of various studies reported that combined treatment showed complications including pain, mucositis, mucosal sensitivity, dry mouth, altered or reduced taste, mucosal and bony necrosis, increased risk of dental caries, difficulty with denture function, altered esthetics, reduced mobility of the tongue, lips, and jaw, and limitation of mastication and swallowing.[20-25]
CONCLUSION
The results showed that the patients treated by surgery alone had slightly better OHRQoL compared with others. In recent years, the management of HNC has been more complex with combined-modality programs, as well as the integration of new diagnostic and therapeutic technologies. The head and neck is the most complex organ, so the treatment decision should best support the patient. The assessment of OHRQoL not only provides information about the impact of cancer and its treatment outcome but the information can also be applied to direct patient care, education, and counseling to optimize physical and psychological well-being.
We recommend further research and awareness among health professionals, patient groups, and policy-makers on whether and how the QoL assessment measures and tools can help patients with cancer.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Pre-treatment performance status and stage at diagnosis in patients with head and neck cancers. Asian Pac J Cancer Prev. 2014;15:8479-82.
- [CrossRef] [PubMed] [Google Scholar]
- Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144:1941-53.
- [CrossRef] [PubMed] [Google Scholar]
- Head and neck cancer burden in India. Int J Head Neck Surg. 2013;4:29-35.
- [CrossRef] [Google Scholar]
- Head and neck cancer: Health related quality of life assessment considering clinical and epidemiological perspectives. Rev Bras Epidemiol. 2012;15:38-48.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical update on head and neck cancer: Molecular biology and ongoing challenges. Cell Death Dis. 2019;10:540.
- [CrossRef] [PubMed] [Google Scholar]
- Oral health-related quality of life in patients treated for oral malignancy at Kanchipuram district, India: A cross-sectional study. Indian J Cancer. 2017;54:11-5.
- [CrossRef] [PubMed] [Google Scholar]
- Oral health-related quality of life: What, why, how, and future implications. J Dent Res. 2011;90:1264-70.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of conventional radiotherapy on health-related quality of life and critical functions of the head and neck. Int J Radiat Oncol Biol Phys. 2006;65:1051-62.
- [CrossRef] [PubMed] [Google Scholar]
- Pretreatment factors predicting quality of life after treatment for head and neck cancer. Head Neck. 2000;22:398-407.
- [CrossRef] [Google Scholar]
- Importance of patient, tumour and treatment related factors on quality of life in head and neck cancer patients after definitive treatment. Eur Arch Otorhinolaryngol. 2009;266:1461-8.
- [CrossRef] [PubMed] [Google Scholar]
- Health-related quality of life as a survival predictor for patients with localized head and neck cancer treated with radiation therapy. J Clin Oncol. 2009;27:2970-6.
- [CrossRef] [PubMed] [Google Scholar]
- Risk for oral cancer associated to smoking, smokeless and oral dip products. Indian J Public Health. 2012;56:57-60.
- [CrossRef] [PubMed] [Google Scholar]
- Oral health-related quality of life in patients of head and neck cancer attending cancer hospital of Bhopal city, India. J Int Oral Health. 2015;7:21-7.
- [Google Scholar]
- Quality of life and recurrence concern in survivors of head and neck cancer. Laryngoscope. 2000;110:895-906.
- [CrossRef] [PubMed] [Google Scholar]
- Health-related quality of life outcome for oral cancer survivors after surgery and postoperative radiotherapy. Jpn J Clin Oncol. 2004;34:641-6.
- [CrossRef] [PubMed] [Google Scholar]
- IMRT for head and neck cancer: Reducing xerostomia and dysphagia. J Radiat Res. 2016;57:69-75.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical features and preventive therapies of radiation-induced xerostomia in head and neck cancer patient: A literature review. Appl Cancer Res. 2017;37:1-8.
- [CrossRef] [Google Scholar]
- Radiotherapy-induced salivary dysfunction: Structural changes, pathogenetic mechanisms and therapies. Arch Oral Biol. 2015;60:1802-10.
- [CrossRef] [PubMed] [Google Scholar]
- Association between general and oral health-related quality of life in patients treated for oral cancer. Med Oral Patol Oral Cir Bucal. 2015;20:678-84.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life and oral function in patients treated with radiation therapy for head and neck cancer. Head Neck. 2001;23:389-98.
- [CrossRef] [PubMed] [Google Scholar]
- Health-related quality of life in long-term head and neck cancer survivors: A comparison with general population norms. Br J Cancer. 2001;84:149-56.
- [CrossRef] [PubMed] [Google Scholar]
- I'm so tired: Biological and genetic mechanisms of cancer-related fatigue. Qual Life Res. 2010;19:1419-2.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life in oral carcinoma: A 5-year prospective study. Head Neck. 2008;30:461-70.
- [CrossRef] [PubMed] [Google Scholar]
- Life after total laryngectomy: A measure of long-term survival, function, and quality of life. Arch Otolaryngol Head Neck Surg. 2007;133:526-32.
- [CrossRef] [PubMed] [Google Scholar]
- Health-related quality of life of head and neck cancer patients with successful oncological treatment. Eur Arch Otorhinolaryngol. 2015;272:2415-23.
- [CrossRef] [PubMed] [Google Scholar]






