Covid associated mucormycosis of the jaw: Expect the un-expected

*Corresponding author: Ganesh Jadhav, Department of Dentistry, All India Institute of Medical Sciences, Nagpur, Maharashtra, India. drganesh2009.aiims@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jadhav G. Covid associated mucormycosis of the jaw: Expect the un-expected. J Global Oral Health 2021;4:129-31.
Dear Editor,
“Fungi make worlds. They also unmake them.” - Merlin Sheldrake
The coronavirus disease 2019 (COVID-19) infection caused by severe acute respiratory syndrome coronavirus 2 has altered the landscape of dentistry in several ways.[1] Due to novelty of the COVID-19 disease, its treatment plan, as well as long term effect of medications on patients, is unpredictable. Wide range of therapeutic protocols of COVID-19 may cause various bacterial and/or fungal co-infections in patients with or without pre-existing comorbidities. Covid associated mucormycosis (CAM), an angio-invasive infection, is one such fungal infection caused by saprophytic Rhizopus species.[2] CAM can be seen in cutaneous or disseminated forms such as gastrointestinal/pulmonary, and rhino-maxillary.[3] CAM is spreading rapidly to cause extensive tissue destruction by the time fungal infection is diagnosed. It shows high mortality rate (50%) that may reach up to 100% in advanced disseminated form in spite of aggressive surgical debridement and antifungal therapy. Rhinomaxillary variant is the most common type of CAM and such patients might visit dental clinics for their intraoral complaints.
Successful management of CAM pose difficulties due to the erratic nature of underlying conditions (Diabetes mellitus, Trauma, Burns, Deferoxamine therapy, iron overload, etc.), distinct pathogenesis (extensive angioinvasion and higher virulence), delay in diagnosis (non-specific clinical manifestations, limited validated serological/molecular methods, and difficulties in culturing organism), restrictions of antifungal therapy (elevated minimum inhibitory concentration of amphotericin B, variable susceptibility of fungus to triazoles).[4] Dental practitioner can play an important role in breaking the chain of CAM in the population by keeping a high level of clinical suspicion in every patient reporting to dental operatory. Dentist must be aware of the warning signs and symptoms of CAM so as to arrive at its early diagnosis to avoid any life-threatening complications. [Figure 1] depicts the Diagnostic Algorithm of CAM. Moreover, dentist can give the following instructions to all those patients who have recovered from the COVID-19 and are reporting to dental OPD.
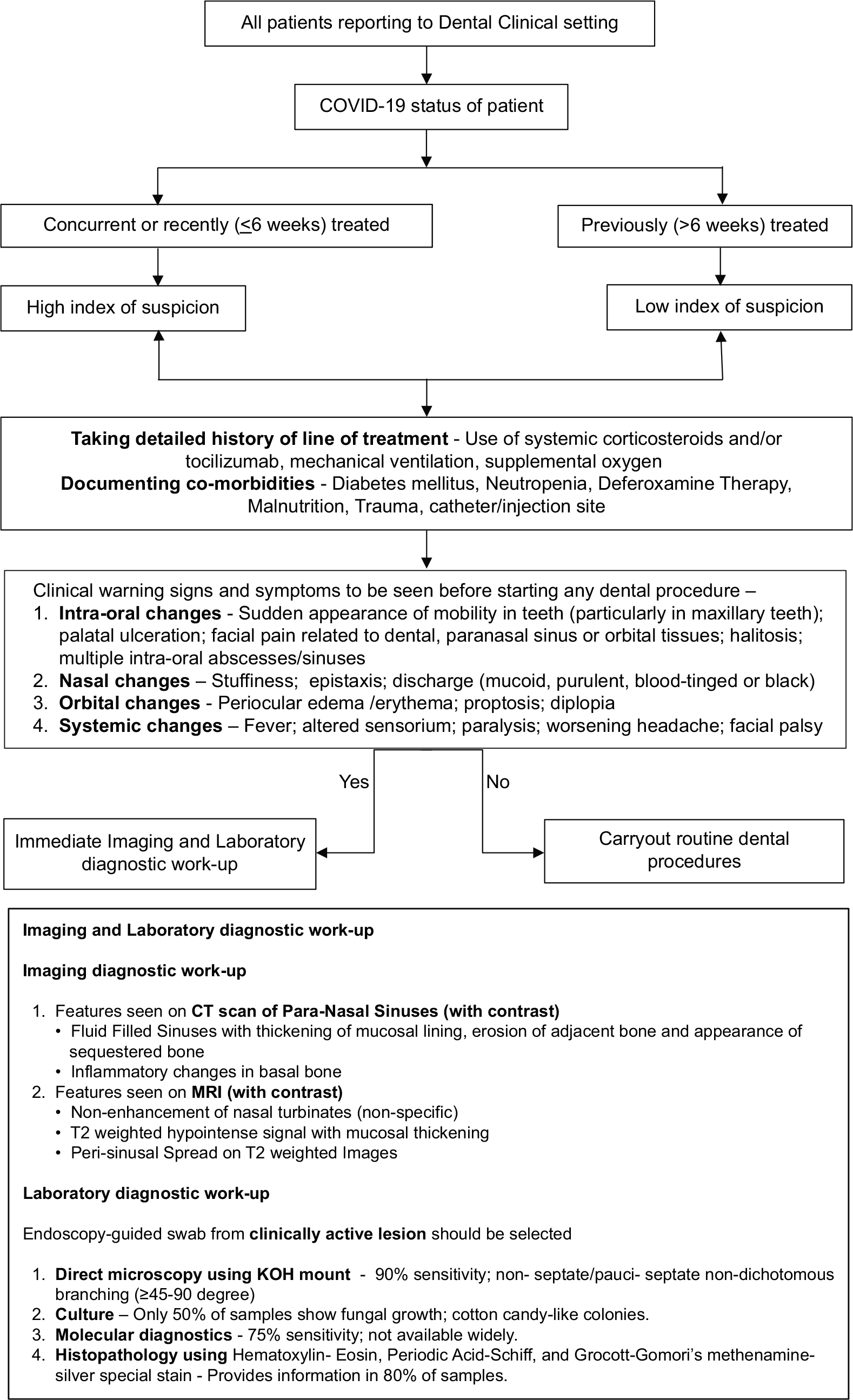
- Diagnostic algorithm of Covid associated mucormycosis.
Careful attention toward the early warning signs and symptoms of CAM for timely reporting
Changing the toothbrush and tongue cleaner post-covid
Oral hygiene maintenance along with routine use of mouthwash such as 2% povidone Iodine or 0.2% chlorhexidine
Steam inhalation for increasing ciliary function to improve the sinus health
Nasal irrigation - 0.5% betadine
The use of multivitamins and low glycemic-high protein diet.
The high prevalence of CAM in the period of modern diagnostic tools demands additional studies as these might help in fighting against this previously uncommon fungus by identifying patient groups that are at higher risk. Instilling a multidisciplinary team-based approach and following a Diagnostic Algorithm is the key to success. Thus, the dental practitioner can be a key player in the management of this fungal outbreak by diagnosing at an early stage with immediate referral, and that ultimately would reduce the high morbidity as well as mortality associated with it. The use of omics for gaining complete insight into the mycoviruses (viruses that infect fungi) therapy is need of an hour.[5]
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Coronavirus disease 2019: Implications for clinical dental care. J Endod. 2020;46:1341-2.
- [CrossRef] [PubMed] [Google Scholar]
- Global guideline for the diagnosis and management of mucormycosis: An initiative of the European confederation of medical mycology in cooperation with the mycoses study group education and research consortium. Lancet Infect Dis. 2019;19:e405-21.
- [Google Scholar]
- Why is mucormycosis more difficult to cure than more common mycoses? Clin Microbiol Infect. 2014;20(Suppl 6):74-81.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology and diagnosis of mucormycosis: An update. J Fungi (Basel). 2020;6:265.
- [CrossRef] [PubMed] [Google Scholar]
- Understanding mucormycoses in the Age of “omics”. Front Genet. 2020;11:699.
- [CrossRef] [PubMed] [Google Scholar]





