Translate this page into:
Practical lessons from a general dentist of more than 50 years private practice plus 2 years of United States Air Force practice

*Corresponding author: T. Bob Davis, Past President of the Academy of Dentistry International, Dallas, Texas, United States. tbob@tbobdavis.com
-
Received: ,
Accepted: ,
How to cite this article: Davis TB. Practical lessons from a general dentist of more than 50 years private practice plus 2 years of United States Air Force practice. J Global Oral Health 2021;4:107-15.
Abstract
Having practiced over 54 years the art and science of general dentistry, many changes in philosophy and performance have occurred. Some are minor while others very major. This series of observations will treat some in detail while others very briefly. The physical locations have been in the Dallas, Texas area of the USA. Definitions of terms set the stage for discussion of the basis of dentistry. Support for the scientific as well as evidence-based approaches is laid forth.
Filling materials have transitioned from amalgam to composite being most prevalent. Fluoride added to local water supplies has decreased the number of decayed/sensitive teeth, the timing of initial decay, and the prognosis for remediation. pH is a major player in the deterioration of tooth structure. New understandings of tooth brushing and oral hygiene have significantly improved the future for continuing dental health. Absence of fluoride in bottled water has taken a front-center stage for helping/hurting chances of keeping teeth free of decay. Fluoride varnishes have widespread acceptance in America. Failure to seek routine dental care has influenced the outcomes for many younger patients, especially those who have graduated high school, gone off to college or into the workforce. Such lack of routine preventive influence raises the costs of care when it is received, often leading to complaints from patients about the high costs of repair. The alternative is prevention with ongoing consistent 6-month recalls/repairs when problems initiate, rather than allowing problems of long duration. The USA dental insurance industry adverse impact on practicing dentists is a vital monologue. Revealing the dental insurance industry as a number one concern of many surveys of practicing dentists is a way of preparing international countries for learning from the flawed USA models. Recent Congressional law, HR 1418, the Competitive Health Insurance Reform Act, will address some of the most critical wrongs by placing the dental insurance industry into antitrust restraints. Current concerns about digital X-ray’s diagnostic potential are revealed. Conservative dentistry is promoted. Results of conservative practice from nearly 50 years are documented with photos and X-rays. Bonded bridge technology is highlighted for its valued impact.
Keywords
General dentistry
Practice management
Conservative dentistry
Preventive dentistry
Dental insurance
Fluoride
Dental legislation
Bonded bridges
Bottled water
Dental philosophy
History of dentistry
Dentistry is considered a science. The word “science” in our English dictionaries is from the root “knowledge” and “to know.” “Comprehension or understanding” with “skill resulting from training” and “special skill” are all listed as what “science” is. “Scientific” is rooted in “to make” and means “well versed in science” and “according to the rules or principles of science.” A “scientist” is “a person versed in or devoted to science.” We may be called “applied scientists” as dentistry is an “applied science.”[1]
Now, it seems to me that we as practicing dentists in daily practice on living subjects (not objects and things) factually live up to those conditions and requirements. We are not subservient to any higher authority in the academia but rather coequals and colabors in the disciplines of the profession of this applied science called “dentistry.” Thus, it implies a requirement that our voices be heard in the scientific dialogue, that our research be as respected as other’s research, and that our experiences have equal weight as to those tangential-to or adjacent-to daily patient care. Clearly, the “evidence-based” conditions that exist in daily practice are as profound as those in the laboratory. It is in that spirit that I offer the following reflections over the past.
Transitioning from amalgam to composite for routine fillings, I began to do more composites than amalgams in August 1974. I have no doubt that composites can last as long as amalgam, if not longer, especially when in small fillings. Composites have been the esthetic choice for facial and facial-cervical restorations from their beginnings. Many have provided long term service [Figure 1].[2] In the early 1970s, a mesial composite on #7, distal on #8, and mesial on #9 were placed before radio-opacity was added as standard [Figure 2]. [2] Adaptic and Concise were brand names. The X-rays look as though there is no filling! For younger dentists that have not seen this early type material, proceed with caution before removing these as they can last decades.

- Facial-cervical composite placed in 1989 (32 years old).
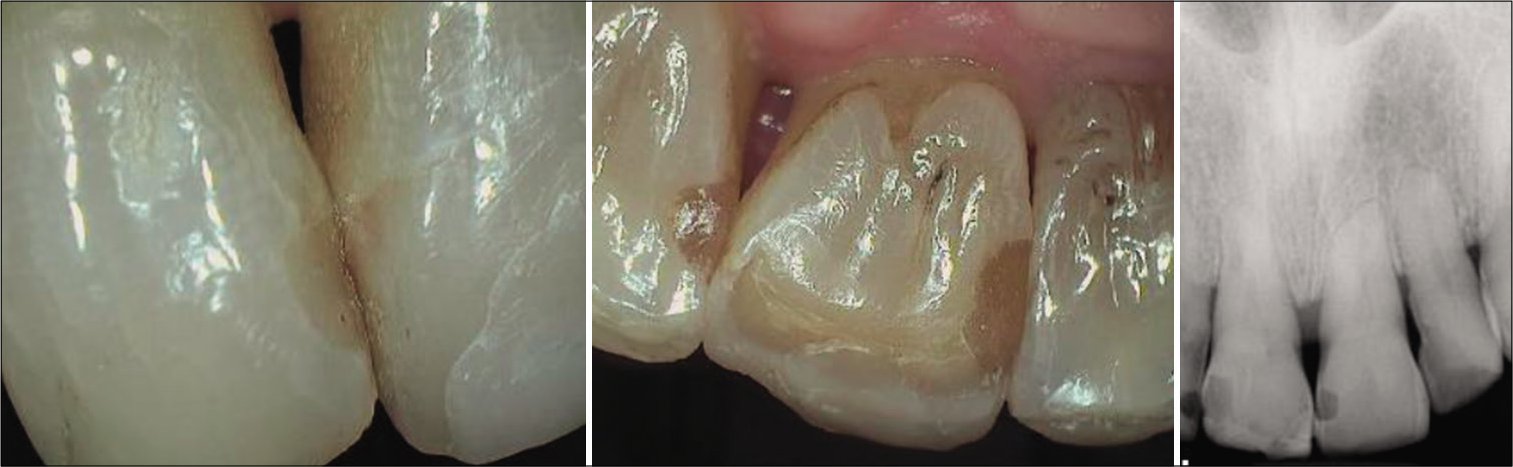
- #7 mesiofacial; #8 distolingual, and #9 mesiolingual. Placed in mid-1970s. Still in service.
With the advent of fluoride in most USA water supplies coupled with varnish use on routine patients, decay is not a major problem in our private practice. Around cervical, a more common problem being additional cervical wear at the enamel/dentin/cementum margins when often no new decay is present [Figure 3].[2] Gingival retraction over time allows more surface root exposure [Figure 4].[2] The issue of abfraction (tensile and compressive forces) is often considered as well as acid erosion (pH lower than 5 or so) and toothpaste abrasives.[3] Adjusting bites and night guard use help abfraction. Acidic drinks like juices and wines are culprits, especially when swished around the teeth. Using a straw may decrease their bad effect. Stomach acid (in reflux disease) has a pH of 1.2 which compares with battery acid’s pH of 1.0. Early diagnosis of reflux with treatment can prevent some erosion. Items such as Vitamin C tablets and mouth mints (cough drops) chewed or held in one area until gone provide rapid dissolution of tooth structure surfaces that are not carious.

- A 13-year successful composite. Apical cervical wear beyond.

- Commonly seen cervical wear.
Periodontist Dr. Mark Glover of Dallas, Texas, was convincingly thorough in a presentation to the Dallas County Dental Society monthly meeting a few years ago pointing to the cause of some abnormal cervical wear at toothpaste abrasives, rather than toothbrush bristle wear.[4] Reflections from his textbook chapter are poignant. First contact toothpaste increases the statistical root damage. Evenly dividing up the toothpaste in all four quadrants decreases probability of abrasive damage. Currently, a pea sized amount of toothpaste is generally recommended. Gel pastes have little to no abrasives and are a good substitute when toothpaste abrasives are starting damage. [4] Much research must be done to adjust the abrasives to meet individual needs, followed by public awareness [Figures 5-7].[2]

- Excessive wear #20 and #22.

- Severe cervical wear.

- Cusp weakened from cervical wear.
The good news from Dr. Glover’s presentation is that toothbrushes do not cause tooth surface wear. Toothbrush use only when toothpaste is not available is also good practice. Missing fluoride and minerals are detrimental to the remineralization of tooth surfaces and allow for more rapid deterioration of enamel and dentin. The presence of lots of healthy saliva with its buffering capacity is critical to surface stability.
Having noticed in my patients during the early 1990s, the relationship between interproximal decay and bottled water, I have alerted our patients of the potential harm of routinely and exclusively drinking water without fluoride. Recent interest in the Journal of the American Dental Association has highlighted the little known problems of lack of minerals in bottled water that leave the human body without necessary and routine minerals for health. “The fluoride concentration in 90 of 92 studied bottled waters is insufficient to contribute to caries prevention…Dental professionals should consider the mineral content of water consumed by their patients during caries risk assessment.”[5]
Fluoride deficient water has led to interproximal enamel demineralization that is becoming more difficult to early diagnose due to the problems with portable handheld X-ray machines/computer interfaces. Clinicians Report (CR) research shows that “most lesions are beyond the ‘incipient’ stage when first identified and would more accurately be classified as ‘small’ to ‘medium’…current caries detectors … provide only limited data on depth, extent, or progression of lesion.”[6] As of late 2020, Christensen states “Digital CMOS X-ray sensors… [currently produce] inconsistent image quality and detail.”[7]
The basic daily routines of toothbrush with toothpaste and flossing are now insufficient. Instead of becoming more capable of early treatment, we have slipped into a time of false assumptions of health. Lurking beneath the hard to touch and see areas are spots already needing preventive intervention. One of the common treatments for such areas is fluoride trays with fluoride gels to be routinely used by patients at home. With such interceptive home care, coupled with routine dental office recall preventive appointments that include use of a fluoride varnish on each recall, many of these incipient lesions may be “arrested.” I was taught the concept of “arrested decay” when in dental school in the mid-1960s. It is still a valid concept today.
In the USA, it is common to see children with little to no decay history until in their late teens. Once they are out from under the normal healthy environments provided by their parents in conjunction with routine preventive dental care from their family dentists, they often go off to college or into the workforce where those routines are lost, not supported, not thought to be necessary or desirable. The sad reality is such short sightedness leads within a few years to a wave of new decay. It is not uncommon for that age group in the late teens and early to late 20s to avoid routine dental habits and appointments for up to 10 plus years. At that point, obvious signs and symptoms appear to the patient with either urgent or painful implications. This puts a burden on the young patient for all at once treatment that is costly up front.
Hindsight could have prevented the conditions and a little payment for prevention all along would have been just a routine small investment in health for a lifetime. By this time, all the hopes and dreams of parents and dental teams are dashed and the dental profession is blamed. These strange and unfounded responses by younger uninformed patients cause conflict with the professionals who are hoping to save their dental health.
It is now an uphill battle with some government programs and insurance plans that try to circumvent existing standard practices in the name of cost containment. The subscriber (patient) believes the insurance company knows their health needs and that the insurance company knows what a fair fee is. Nothing could be further from the truth. It is often a cover for forcing the patient to choose less quality care or, in confusion, thinking if insurance does not cover that procedure it must not be needed.[8] These unexplained, asterisk footnoted, in small print, paper notified issues, sent after the fact of denial, often alter the doctor/patient relationship, causing grief to the patient and practitioner. This is classic “interference with the doctor/patient relationship” that has been hallowed from the beginning of dentistry.
The so-called “insurance industry” of the USA is of little help in encouraging patients to be preventive oriented. Insurance industry personnel do not call or contact their clients at the client’s point of need of that care nor for early intervention for dental disease. They do not provide an immediately available client assistance expert at the point of receiving their treatment plan who can immediately answer their questions necessary for decisions based on insurance participation. This is the basic total failure of the “dental insurance industry” in the USA! Their desire for sales and profit overrides the basic opportunity to offer a preventive service ongoing for such young people out on their own or for clients of any age.
“Dental insurance” is a misnomer since it is only actually a poorly designed money management scheme. It has no inherent “insurance” of dental success! Factually, it is a false and misleading concept that asserts “insuring” – which is a synonym for “assuring and guaranteeing.” No good end results when the dentist is left to explain the failed promises of the policy that is too little, too late, too unexplained to patient by salesmen or employer’s representatives. Their product is a part of a benefit package, as individual policies are uncommon, and not a true insurance product. It is a middleman attempt to money manage both entities, dentist and patient. How can they live with most all surveys of the USA dentists in the past decades reporting the number one problem in dental practice is “dental insurance?”
Patient directed anger at the dentist should be placed at the feet of the so-called “insurer” who has literally, by not informing, allowed the patient to believe (assume) that which is not true (that they have money to take care of all their dental needs). It is so common to hear a newly insured patient to announce to me “I now have insurance and can get all my teeth fixed.” They so often say “I have $1000 (or whatever the limit is) to pay you.” Clearly, they have had no prior discussion with insurer/employer of deductibles, copay, outdated area averages-per-procedure that were used to set fee schedules, exclusions, extractions before initiation of the policy which deny a replacement, and a myriad of other in-small-print conflicts with getting the whole amount; no awareness that the insurer does not guarantee payment of a pre-determination; no awareness of problems associated with double coverage (i.e. wife/ husband). No discussion with their client (our patient) is offered by insurance salesmen (or by employer purchaser of group policies) of the reality of costs of delayed dental care and disease remediation. Delays in processing a simple clean claim can take weeks; a one issue conflicted claim can take months. How did that come about?
It happened in the late 1960s and early 1970s when dental insurance plans began. I had just started private practice and saw them begin. The basic benefit then was $1000/year with the premium to represent what it cost to do that business. Strangely, today, the most common dental insurance policy provides only $1000 of benefits.[9] It is obvious the premium are not the same, the benefits are non-relevant to current costs for providing the same dental services, and the insurer has no demonstrated process for their client to have real-time/on-site help from insurer at point of need time (their appointment when a treatment plan is presented). The benefit may not have been referenced by the insurer to represent any valid update in annual costs of dental care, with questions of comparisons of costs in rural versus city, one state versus another state. The patient has no access to those basic building blocks or incorporation of latest technologies.
Too often, my business manager must spend up to hours on hold by phone with an insurer inquiring as to the validity of the patient’s insurance being current, the details of coverage of treatment plan items, and the innuendos of exclusions/already used funds or secondary insurance challenges! Add to that the all too routine of claims being denied over a technicality that the patient or insurer could/should correct, not the dental office personnel. Yet, the insurer literally never contacts their client and the client rarely contacts the insurer to resolve those sales/ client questions/discrepancies/typo’s/non-clean paper/electronic claims. This costs the dental office a substantial overhead that is not reimbursed in any form by insurer or patient.
The problem lies at the feet of employers who want to do something for their employees but are willfully uninformed as to the realities of dental reimbursement. The dental insurance industry has not taken inputs from the profession regarding the need of the hour. I know from personal experience having tried to negotiate with a former colleague who headed up one of the largest dental insurance companies in the USA! Having been in leadership positions, I know from personal experience the huge difficulties of getting an audience with those who plan/sell/provide as a benefit dental insurance. Money speaks louder than ethics and humanitarian causes.
The dental profession must demand ethical practice from the dental insurance industry regarding the needs of our patients. USA Federal Law HR 1418, the Competitive Health Insurance Reform Act, of January 2021, is thought to provide relief and leveling of the playing field for dentists. Time will tell!
Concomitantly with the concept of solving the dental health needs of patients is a concept of prevention of disease and minimizing the surgical and restorative needs of all patients. That is a concept my generation started out in dental school believing was our mission in life. To our credit prevention is possible, early treatment is available and lasting restorations continue to improve overtime. The inlay/onlay photos [Figures 8 and 9][2] confirm that gold restorations can average 40 years of life expectancy, as reported by Dr. Christensen.[10] Note the conservative preparations. It is noteworthy that he also reports porcelain fused to metal crowns can average 20 years in service. As of this writing, the new zirconia crowns are passing the 12th year of documented existence. Longevity of restorations is both an economic and health benefit for patients. We seek total societal cooperation in working together toward prevention and health for a lifetime.

- (Still in service). Gold onlay #19 seated 1972 (49 years old). Gold onlay #19 seated 1972 (49 years old).

- (Still in service). Gold onlay #30 seated 1989 (31 years old).
One of the concepts of today’s dentistry is to provide conservative restorations. Yet, most of the world of dentistry has not embraced the reality available already! An example that I hold close to my practice and life is the concept of minimally invasive long-term bonded metal-to-porcelain bridges [Figures 10-13].[2] It is a concept that has great success but little understanding by practitioners, little utilization by general dentists or prosthodontists. Gordon Christensen states that “Millions of these restorations are placed each year with only a small percentage of failures at 5 years and 70–80% success at 15 years.”[11] My personal journey with that technology has allowed me over 200 cases spread over 39 years. They are less costly than any other bridge, requiring minimal preparation of enamel, non-invasive, generally done without local anesthesia, and accomplished in a couple weeks for laboratory fabrication. As of this writing, the allporcelain/all-zirconia-based wing style attached bridges have yet to meet expectations due to breakage and amount of preparation needed.

- (Still in service). Seated 1982. (38 years old – never debonded).

- (Still in service). Seated 1985. (36 years old – never debonded).

- Seated 1988. (28 years service). (Patient deceased).

- (Still in service). Seated April 29, 2008. A 13-year success.
An American Dental Association Journal article by Limones et al. reports “the use of MC FPD (Metal to Ceramic Fixed Partial Dentures or Bonded Bridges) should be considered first for the posterior sector, in which esthetics do not seem to be crucial…”[12] My experience documents good anterior and posterior survival rates of over 30 years without debond. Approximately 60% of mine are posterior bridges. The great materials and laboratory processes that lead to dozens of years success with such inexpensive bridges have saved many patients initial excessive costs and invasive procedures that often require later replacement with more excessive costs and invasive procedures.
With many studies that validate the acceptability of working on patients even with high blood pressure and elevated heart rates,[13] it is a common option in my practice to offer fillings without anesthesia. This is especially effective with fillings for young children on whom we place headphones with music (sometimes offering nitrous oxide alone or concomitantly with the headphones). I quickly note that parents and caregivers are allowed in the operatory but not allowed to speak nor be physically contacting patient, that is, holding patient’s hand or making child feel dependent on parent rather than being a self-responsible person. This also teaches the young patient while reassuring the parent they can accept routine dental care on every future visit. To not use a needle nor leave the patient with numbness at the end of appointment is a highly valued concept by both patient and parent! Frankly, this option works best on children of parents who have earned the respect of the child in what the parents say and do. Disciplined children are great patients!
It is a common option in my practice to offer other procedures such as crown and bridge preparation and large fillings or most bonding of single surfaces without local anesthesia. It is highly effective with a large percentage of older patients whose tooth mineralization is very high, especially in the fluoride-rich environment of many (water, food, daily toothpastes, fluoride rinses, and office placed fluoride varnish). Most who accepted the offer (including the younger generations) will at the end express deep appreciation for not using the needle/local anesthesia due to the numbness, or tingling during recovery.
Naturally, if sensitivity occurs during a procedure, it is easy to place local anesthesia before continuing. It goes without saying that a previously done crown prep on teeth that have been treated with root canals and only needs touching up for making a new crown (especially on teeth that have had crowns cemented for years that have become dislodged) are perfect candidates for such postponing local anesthesia until or if needed.
Remarkable success is achieved in our office on an occasional root canal treatment without anesthesia when the tooth tests completely dead and non-responsive. I understand that a needle injection opens a new wound through tissues already generally swollen and infected. It then allows deposit of liquid that quickly starts pressure pain which requires time to be decreased. At the same time, the infected/inflamed tissues are pushed around and mixed with the foreign liquid which then causes more inflammatory response, totally unneeded but shocked into existence, forcing liquids beyond the infected area most likely. The body and mind are having to deal with all that plus the worry of what you might be doing within the confines of the tooth.
With that process potentially compromised due to inflammation, why would a dentist choose to insist on local anesthesia when there is likely no basis for pain while inside the confines of that tooth? First, a valid pulp test should be performed that indicates no nerve transmission. Second, a reassurance that we will quickly give anesthesia if any pain is felt. Third, careful entry to the apex with ample and routine irrigation and files to appropriate size. Such good technique including irrigation with chlorhexidine gluconate (water based)[14] after distilled water has proven in our time to be significant in decreasing post-operative swelling and trauma pain. Patients are notified in advance that it is nothing more than awareness and not pain. They may feel a slight warmth as the warm gutta percha is placed. Such patients routinely thank me for not using the needle.
Add to that process the reality that the acidity of the abscessed area has another acidic liquid called local anesthesia forced into it. “Local anesthetics… (pKA averages 7.7–8.1 in current use)…containing vasoconstrictors are acid solutions…when inflammation is present, tissue pH becomes more acidic and local anesthesia is more difficult to achieve…injecting through areas of active inflammation is to be avoided…”[15] When common sense and good judgment prevail, we realize the contraindication for local anesthesia for these totally non-responsive teeth. It also allows for treatment in all four quadrants in one appointment without our concern for how many carpules are safe in one appointment.
Consider the timing of the onset and recovery of such local anesthesia; “…pain fibers are blocked first, followed by temperature, touch, pressure, and motor function…the onset of an inferior alveolar nerve block is therefore proximal to distal, molars to incisors, and lower lip. Recovery is also proximal to distal, with the lip being the last to recover from the block.”[15] Avoiding this uncomfortable period of time is very patient friendly. For children, the decreased possibility of biting lips or cheeks is significant. The lingering effect (and uncommon delayed recovery) is a significant bad memory for children and adults and is a leading cause for not returning for treatment.
I routinely personally call all my root canal and oral surgery patients the evening of the procedure to hear their experience between the appointment and near bedtime. In advance, we offer them a recommendation of ibuprofen alternating with acetaminophen every 4–6 h post-operative. In general, we have them take the ibuprofen first dose in the office at the beginning of either an endodontic or oral surgery appointment. It has been my observation that those endodontic patients without local anesthesia outperform postoperatively those who used local anesthesia. This is a challenge for some long-term research into this obvious option of limiting local anesthesia use.
Rarely does a patient “need” antibiotics unless in the presence of pronounced swelling/inflammation.[16] The current concerns with Clostridium difficile adverse outcomes negate the cavalier use of antibiotics in general. Likewise, rarely if ever does a patient “need” a narcotic for a dental procedure.[17] Use of narcotics for such unwarranted cases has led to the most horrific of addictions. Wisdom had been swapped for convenience of practitioner and desires of patients. Ibuprofen (NSAIDs) and acetaminophen have proven track records of better, safer, and more effective pain relief without the severe consequences of opioids.[18]
As a matter of quality control, I have from the beginning of my private practice used non-resorbable sutures for surgical procedures.[19] My basis is I wish to see the end result of all my surgeries, routinely at the 7th or 10th day post-operative. This is highly instructive for me as a practitioner. I can understand what is common or uncommon as a consequence of such a surgery. I can tell future surgery patients what to expect in the recovery time, offer wise pre-operative/postoperative pre-printed instructions, allay fears, and assure the patient’s body is prepared for the surgery. I propose having the patient’s nutritional condition excellent at point of surgery is of significant importance for post-operative healing. Practical experience over these decades has proven this value-added pre-operative preparation.
Consistent with current best practices, we have taken/ recorded vital signs on every patient, at every appointment.[20] Thus, we have been timely in referring dozens of patients whose vital signs are in crisis, before our treatments, to the appropriate medical doctor/hospital.
These concepts beg the need for ethical practitioners who hold the line on prescribing and diagnosing. Overdiagnosing is a growing problem in the USA as the capacity to do procedures overwhelms the ethics of some practitioners who feel the need to do what they are capable of doing regardless of the value/necessity/appropriateness to the patient. State Board of Dental Examiners is in place to protect the public but seldom do these cases reach that level until there is some radical crisis. Ethical norms are at best difficult to monitor because no other practitioner sees the work of such overdiagnosis/overtreatment until it is generally too late. Third-party involvement is often skewed in the name of data interpretation that is easily misinterpreted.
Meanwhile, a few bad actors continue to get away with less than acceptable care. We have all seen before and after cases in the printed literature and lectures that make a conservative dentist uncomfortable with the minor changes considering the extensive procedures and costs with questionable longer term success than if left as is.
One of the long-held concepts taught to me in dental school was the idea of not putting crown margins closer than 2 mm from the bone. In the new age of fluoride, brushing and flossing, water irrigation, interproximal brushes, and office-based care, I have long disagreed with that thesis. Note the excellent results of such a case over the past 12 years, with no hint of breakdown. I have seen this many times [Figures 14 and 15].[2] So do not be fearful when this deep margin is needed. Just make sure the patient practices all the previously detailed preventive measures.

- Seated June 30, 2009.

- January 28, 2021. Note: No bone loss.
Sensitivity seems to be a much talked about issue in the dental literature. In my practice, we often find one single sensitive tooth relates to biting/chewing/clenching/grinding trauma. A small occlusal touch on a heavy contact by a slow speed round diamond may bring a quick response. Checking lateral excursions may identify the offender, that is, balancing interference or tendency toward group function.
The uncommon facial cervical sensitivity is treated with commonly available desensitizing liquids or home use gels. The heavy grinder will often show worn cusp points. The clencher may have one sore tooth and/or some tori formation. In today’s more stressful work and living environments, we are seeing more clenchers and grinders. They are best treated with night guards, most of which are placed on the maxillary teeth. Sensitive other tooth surfaces are now uncommon in my practice.
Fluoride was added to the Dallas water supply in 1967, my 1st year in Texas. The fluoride generations seem to be less bothered by surface sensitivity. Our use on all recall appointments of fluoride varnish intercepts much of it. We rarely see a sensitive filling. My explanation is our routine use of a liner (Vitrebond)[21] under all fillings where dentin is evident. I also have stuck with one bonding filling material through the years with the occasional upgrade by the manufacturer (generally with a name change). In the past decade or so I rarely will use liner under facial or cervical repairs. I have stuck with the so-called 4th or 5th generation bonding technique, but never mixed and matched different brands of primer/bonding liquid/composite, and never tried the one step 3-in-1 materials.
I continue to do a lot of bulk filling. My chairside staff and hygienists practically never hear of any just seated sensitivity of a crown as I most often seat crowns without anesthesia and would know immediately if one were to be sensitive. I relate this success to brand loyalty due to good results.
The argument of using live patients on state board examinations is being generally dealt with since the American Student Dental Association along with the ADA passed policy at the turn of the millennium to cease the practice, now 20 plus years in the process.[22] COVID-19 has certainly contributed its share of impact on that issue! Time will tell whether the newly chosen alternatives will adequately identify all those ready for license.
Noticeably, the overall percentage of solo private practice general practitioners is shrinking with an increasing percentage of new dentists joining group practices, mostly based on the large average school debt that demands repayment in a timely manner. This seems to beg exclusion from buying a solo private practice in lieu of making immediate progress on paying down the school loans. This has stoked the need for older private practitioners to stay in practice longer, while waiting for someone who will buy the practice. Many do not want to sell to a corporate entity fearing outside influence on the dental care given.[23] State laws and national organizations seek to protect the public from non-licensed dentist diagnosed treatment plans.
With the increase in marketing by many of the home dental health supply companies, much by flashy commercials on TV and in print media, dentistry has been helped at getting daily prevention out into the public square. Now, the cost of such prevention is more in line with other items people readily buy for themselves in their “wants” category. An example I offer patients is the daily investment of their disposable funds on coffee, soft drinks, cookies, candies, popcorn, bottled water, energy drinks, alcohol, etc. Most of these daily expenditures ($3–$8 USD) amount to a significant annual outlay. Swapping these pleasures (that are often detrimental to good dental health) for excellence in dental routine care can often amount to upward of over $2000 (USD) per year (an amount once promoted as the average annual dental cost per patient in the USA.) When people say that they cannot afford regular dental care, they are often ignoring this hole in their financial dike.
This partnership with the dental supply/manufacturing industry has helped change the public “need” toward a public “want.” Only when people really “want” something will they be willing to work to “pay for” it. It is conclusively true that “until the public wants lifetime dental health” the problem of dental care still being a “dental disease model” is our liability and challenge for the future!
Should the public begin to choose wise dental health daily options, the need for dental repairs will decrease. As we enter 2021 full of hope and expectations of COVID-19 and newer strains getting under control, we can plan ahead for excellence in our patient care.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The New Webster Encyclopedic Dictionary of the English Language Chicago: Consolidated Book Publishers; 1970.
- [Google Scholar]
- Periodontics: Medicine, surgery and implants In: Glover ME, ed. Periodontal Plastic and Reconstructive Surgery. Vol Ch. 21. St. Louis, Missouri: Elsevier Mosby; 2004. p. :413-8.
- [Google Scholar]
- An Investigation into the potential anticaries benefits and contributions to mineral intake of bottled water. JADA. 2020;151:924-34.
- [CrossRef] [PubMed] [Google Scholar]
- Momentum Insurance Plans INC., Annual Maximum (Benefit) Available from: https://www.momentumplans.com/dentalinsuranceglossary/annualmaximum
- [Google Scholar]
- Future of Dentistry Chicago: American Dental Association, Health Policy Resources Center; 2001. p. :14-5.
- [Google Scholar]
- Replacing a posterior tooth with a three-unit fixed prosthesis-help with your difficult decisions in 2011. Clin Rep. 2011;4:2.
- [Google Scholar]
- Zirconia-ceramic versus metal-ceramic posterior multiunit tooth-supported fixed dental prostheses. JADA. 2020;151:230-8.
- [CrossRef] [PubMed] [Google Scholar]
- Canceling dental procedures due to elevated blood pressure. Is it appropriate? JADA 2020. ;. ;151:239-44.
- [CrossRef] [PubMed] [Google Scholar]
- Chlorhexidine Gluconate Oral Rinse USP 0.12%. Alcohol Free. Sunstar, G-U-M. Sunstar Americas, Inc;
- [Google Scholar]
- Pharmacology of local anesthetics used in oral surgery. Oral Maxillofac Surg Clin North Am. 2013;25:453-65. vi.
- [CrossRef] [PubMed] [Google Scholar]
- American College of Emergency Physicians Endorses Association's Antibiotics Guideline. Vol 51. ADA News; 2020. p. :15.
- [Google Scholar]
- Increased opioid prescription fills after dental procedures performed before weekends and holidays. JADA. 2020;151:388-98.
- [CrossRef] [PubMed] [Google Scholar]
- Case Western Reserve University Ibuprofen, Acetaminophen more Effective than Opioids in Treating Dental Pain. 2018. Available from: http://www.sciencedaily.com/releases/2018/04/180417181101.htm
- [Google Scholar]
- What every dentist should know about oral mucosal wound healing. Gen Dent. 2020;68:24-6.
- [Google Scholar]
- Wherever you are Today you won't be there Tomorrow. 2019. https://www.levingroup.com/wp-content/uploads/2019/09/wherever_you_are_today_white_paper.pdf
- [Google Scholar]






