Translate this page into:
Tobacco control in India: Enforcement strategies and challenges

*Corresponding author: Dharmashree Satyarup, Department of Public Health Dentistry, Institute of Dental Sciences, Siksha ‘O’ Anusandhan Deemed to be University, Bhubaneswar, Odisha, India. dharmashree_s@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Satyarup D, Kumar M, Dalai RP, Bal SC, Panda S. Tobacco control in India: Enforcement strategies and challenges. J Global Oral Health 2022;5:119-3.
Abstract
This paper focuses on the various legislations passed by Government of India to curb the sale and use of tobacco products. The laws have gotten stricter with every passing day and enforcement has also tightened. However, still a vast majority of the Indian population continues to use tobacco. Hence, more efforts need to be directed to limit this menace.
Keywords
Tobacco control
Tobacco laws
Challenges
Tobacco use
INTRODUCTION
India is the world’s third largest producer of tobacco and its second largest consumer.[1] Tobacco in India is consumed in both smoked and smokeless form but the burden posed from use of smokeless form exceeds that of smoked form.[2] 266.8 million Indians are found to practice some form of tobacco use.[3] Although the use of tobacco poses a significant public health concern, control of tobacco use is complicated by its contribution to commerce.
INCEPTION
Steps to control tobacco use in India have been growing steadily with various legislations passed by the Government of India. The beginning of tobacco control in India started with enactment of the Cigarettes Act in 1975.[4] It was made mandatory to issue statutory warnings on cigarette packets according to the Prevention of Food Adulteration. States such as Karnataka and Maharashtra prevented smoking tobacco in public places. The warning had to be 3 mm regardless of the sizing of the branding and printed in English and also in the same language as the branding. However, this was specific only for cigarettes and did not include other tobacco products including chewable tobacco. Smoking of tobacco was included in the Prevention and Control of Pollution Act in 1981. Smoking and spitting in public transport was prohibited under the Motor Vehicles Act of 1988. The Central Government, in 1991 amended the Cinematograph Act that prevented facilitated smoking in films. Next under the “Drugs and Cosmetics Act” in 1992, toothpastes and toothpowders were banned from incorporating tobacco products in them. In 2000, Cable Televisions Networks Amendment Act considered advertisement of tobacco products by electronic media punishable.
Apart from these nationwide efforts, individual Indian states have tried tackling use of tobacco through state legislations. The first state to ban smoking in public places was Delhi in 1996. Furthermore, sale of tobacco products within 100 m from education establishments and to minors was punishable. Similar anti-tobacco laws were passed in other states such as Kerala and Goa in 1999.[5]
A new Cigarettes and other Tobacco Products Bill was proposed in 2001 under which health warnings on all tobacco products in English and local language was mandatory, smoking in public places was prohibited, and sale of tobacco products to minors was punishable. It also discouraged sport events being sponsored by tobacco companies and advertisement of tobacco products. This came to be known as Cigarettes and Other Tobacco Products (Prohibition of Advertisement and Regulation of Trade and Commerce, Production, Supply and Distribution) Act, 2003 (COTPA) that is an all-inclusive Indian law concerned with control of tobacco. Punishment for defying these legislations was also more harsh.[6]
Further measures discouraging smuggling and levying higher taxes on tobacco products have also been implemented. Taxes contribute to 55% of the cost of cigarettes, but taxes on bidis are much lesser and small local companies manage to evade these taxes. This leads to fall in the purchase of cigarettes but offers cheaper alternatives especially for those in the rural regions of India. However, still the World Bank expects a fall of 8% in the developing countries with an increase taxes by 10%.[5]
After Government of India endorsed World Health Organization Framework-Convection on Tobacco Control (WHO FCTC), focus was on reducing the supply of tobacco and tackling demand. However ultimately, success of tobacco control legislations depends on availability of a competent enforcement setup.
WHO’S TOBACCO-FREE INITIATIVE
The WHO in 2008 introduced MPOWER that comprised six high impact but cost effective measures to combat use of tobacco as a part of its FCTC agenda. At present, 40% of world’s population and more than half of the countries have put into action a minimum of one of the measures put forth by MPOWER. The following are the measures advocated by MPOWER:
M – monitoring use of tobacco
Data are required to evaluate and implement successful anti-tobacco policies. Hence, countries who are party to FCTC are required to continually monitor patterns, determinants, magnitude, and consequences of using tobacco. Monitoring and collection of data should be done using scientific standard and evidence-based methods. The Global Adult Tobacco Survey (GATS) was undertaken in India for the 1st time in 2009–2010 and then again in 2016–2017. It used a multistage sampling technique to include those aged 15 years and over through household survey.[7]
P – protection of people from tobacco smoke
Exposure to tobacco smoke is known to cause various diseases such as cancer, heart diseases, and even death in non-smokers. Passive smoking is known to kill more than 1 million people worldwide every year and especially poses a higher risk to children and newborns. FCTC advocates creation of smoke free zones in workplaces and public places. Completely banning smoking indoors have been proven to protect from the harms of passive smoking and also considerably reduce smoking among adolescents.
O – offer aid to quit use of tobacco
Most tobacco users are unaware of its harmful effects and health risks. Advise and counseling from health professionals can aid in quitting tobacco habit. Use of medication along with counseling is known to increase the chance of quitting by double. FCTC mandates establishment of tobacco cessation systems by all governments. Training packages and capacity building material are provided by the WHO. It advocates success of tobacco cessation through integration into existing primary health-care systems, introduction of mCessation, and setting up of national toll-free quit lines.
W – warning regarding the dangers of tobacco
Smoking and chewing of tobacco causes extensive damage to the body but most tobacco users underestimate these harms. In addition, attractive packaging and advertising of tobacco products distracts its users from the real harm caused by them. Article 11 of FCTC provides guidelines on including health warning on tobacco products to discourage its use. This along with anti-tobacco drives and awareness campaigns are found to reduce tobacco use.
E – enforcing bans on advertising, sponsorship, and promotion of tobacco products
In general, use of tobacco is associated with glamour, success, and being trendy. This is the result of competent and successful advertising of tobacco products. Tobacco industry is worth billions of dollars and, therefore, tries to lure consumers through glossy advertising into often a lifetime of addiction. Article 13 of FCTC proposes complete ban on advertising and sponsorship associated with tobacco. The WHO strongly pushes for a complete ban as otherwise it could lead to mushrooming of other small local tobacco products. When restriction is done effectively, it is known to reduce use of tobacco considerably especially among youth.
R – raise taxes on tobacco products
Article 6 of FCTC calls for increasing excise taxes on tobacco products. Raising costs of tobacco products will discourage its use, especially by adolescents and those from lower income groups, in whom actually the use of tobacco is high. The WHO proposes this measure as one of the most cost-effective method of cutting tobacco use. An increase in taxes saves the health-care sector millions of dollars that would otherwise be spent on providing long-term health care to tobacco users.[8]
NATIONAL TOBACCO CONTROL PROGRAMME (NTCP)
To fortify the enforcement of tobacco control under COTPA and WHO FCTC, Indian government launched NTCP in the year 2008. It was a nationwide program that had first ever funds allocated at state and central level for provision of tobacco control. This aimed to establish tobacco cessation centers (TCCs) all over the country, provide training to available work force such as health care workers and teachers in tobacco cessation counseling. Endeavors to increase public awareness to bring about behavior changes, setting up laboratories for tobacco products testing, training and research for alternative crops to tobacco cultivation, and surveillance of tobacco usage through GATS was also undertaken under this program. It was supposed to be a top to bottom approach with execution of the program at three levels; center, state, and district levels but execution and penalty for violations were unable to be carried out efficiently due to lack of infrastructure and workforce.[4,9] Resource Centre for Tobacco Control (E-RCTC) has been started as a joint initiative of PGIMER (Chandigarh) with the union that aims at compiling and disseminating information and to act as one-point resource system for all tobacco-related activities across the country. It has various IEC materials and provides information regarding training and research related to tobacco control.[10]
SETTING UP OF TCCS
For the current users of tobacco, the only way out of mortality and morbidity associated with tobacco is through counseling to quit the habit. To aid users of quitting tobacco, Ministry of Health in partnership with the WHO FCTC in 2002 initiated setting up of 13 TCC all over the country in varied settings such as psychiatric hospitals such as NIMHANS, cancer, chest, cardiology and surgical hospitals, medical colleges, and NGOs. Their main objective was to create awareness on tobacco cessation while providing training [Figure 1]. They conducted awareness campaigns in the community, especially in vulnerable regions such as colleges, schools, slums, and work places. At Ministry of Health and Family Welfare in Nirman Bhawan, a model TCC for workplace was set up. These were then developed into RCTC in 2009 that provided assistance to other institute to establish TCC.[4]
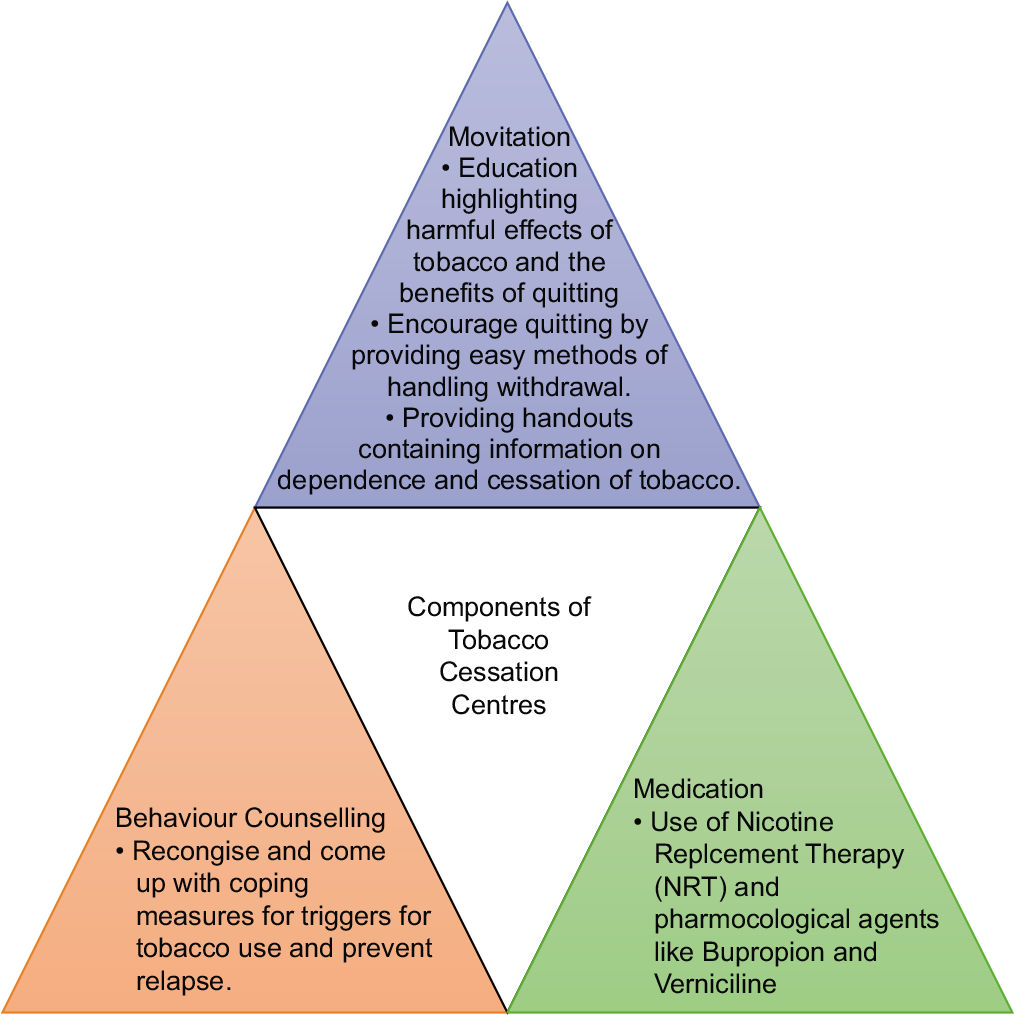
- Components of tobacco cessation clinic.
The centers are managed by staff comprising a medical officer who has been trained in a 2-day workshop in pharmacological and psychological management of tobacco cessation along with a psychologist and social worker. Each center is equipped with a carbon monoxide monitor, a computer, and two personnel. The centers maintain a follow-up of a minimum period of 6 weeks and aim to maintain longer follow-ups. Their work is reviewed through an annual meet and also boosts their expertise through workshops. Endeavors such camps, awareness events through community participations are used to reach tobacco users from slums, colleges, etc.[11]
However, the main set back of these setups was that the reach was limited to those who visited these centers and was not available to most rural residents.[12]
ESTABLISHING TCCS IN DENTAL COLLEGES
To increase the reach of TCCs, dental colleges across the country were required to set up TCCs in accordance with the Dental Council of India guidelines 2018 [Table 1]. A TCC is defined as fixed premises where qualified health-care professionals/counselors provide tobacco cessation therapy for all forms of tobacco by helping patients in their attempts to quit their habit. This could be done through individual or group counseling that may or may not include pharmacological therapy if the TCC is registered to do so. These centers aimed to deliver tobacco cessation services to the patients with tobacco habits that included providing telephonic reminders, self-help information, and interaction with other users who quit tobacco. The TCC also conducts community awareness campaigns by organizing mass awareness programs in schools, colleges, etc., providing training to school teachers or primary health care workers, design and develop education and information material, and conduct oral screening and cessation programs with the aid of Mobile Dental Units. TCCs also act as a center for collection of data and conduct research to evaluate the different cessation modalities and to discover innovative methods.[13]
| Expanding reach to larger populations | Presence of 310 dental colleges in India assures reach to vast majority of the population. Rural regions too can be accessed through community awareness programs conducted by the dental colleges |
| Use of existing trained health personnel | A dental professional employed in dental colleges spends a considerable amount of time interacting with the patient while eliciting case history and establishing diagnosis. This valuable interacting with the patient can be used to identify tobacco habits and initiate to quit the habit |
| Availability of competent platform for follow-up | The inherent recall protocol required for most dental treatments can be used to follow-up on quit strategy suggested to the patient |
| Opportunity to sensitize future dental professionals | Inclusion of tobacco cessation into dental curriculum would also assure training and sensitization of future dental graduates |
The WHO’s Tobacco-Free Initiative celebrates World No Tobacco Day on May 31 of every year. Messages and themes reflecting anti-tobacco policies are highlighted and celebrated on this day. The activities surrounding the theme are organized by TCCs with the cause of public awareness being given high priority.[4]
M-CESSATION PROGRAM:
The deficiency in reach of established TCCs, especially in the rural and suburban areas, can be overcome by the use of mobile technology.[14] Government of India in collaboration with WHO and International Telecommunications Union has adapted a cessation program to be used over mobile phones that works on the WHO’s “Be Healthy Be Mobile” initiative. This mCessation program is for those who are looking forward to quitting tobacco. Giving a missed call on 01122901701 will register the user to the quit program who will receive a Short Text Message (SMS) from 5616115, following which, user will receive 150 SMS that are tailor made to the user supporting them in their endeavor to quit tobacco. The program custom designs the intervention based on the user’s planned timeline for quitting and specifics about the tobacco habits and degree of dependence. According to the Government of India website, over 1 million users have registered for the program and have experienced 19% quit rates observed at end of 30 days.[15]
Novelty of this program is that it provides support targeted to overcome the challenge of quitting tobacco use. The mCessation program is available English and Hindi language and it is deemed very cost efficient as it does not require internet connection and can be availed free of cost. From September 2018, the national tobacco quit line is also available in South Indian languages and has received over 5 lakh calls. It is monitored by NIMHANS and those who are unable to quit with only aid of quit line are referred to the nearest TCC.[16]
CONCLUSION
The Ministry of Health has introduced many steps and passed legislations to control the use of tobacco products. However, the success of these legislations falls squarely on the shoulder of the public and civilians as, it is their stringent behavior that determines their execution. Furthermore, as a public health dentist, it is our social responsibility to protect and to report tobacco violations, as is our obligation to educate and create awareness regarding harmful effects of tobacco use. Working together we can curb the trade of tobacco products and bring about a remarkable achievement in terms of political will.
Declaration of patient consent
Patients’ consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- The Tobacco Atlas. 2012. (4th ed). Atlanta, GA, New York: American Cancer Society, World Lung Foundation; Available from: http://www.tobaccoatlas.org/uploads/Images/PDFs/Tobacco_Atlas_2ndPrint.pdf [Last accessed on 2022 Jun 17]
- [Google Scholar]
- Ministry of Health and Family Welfare, Global Adult Tobacco Survey, India New Delhi: Government of India; 2010.
- [Google Scholar]
- Tobacco control policies in India: Implementation and challenges. Indian J Public Health. 2011;55:220-7.
- [CrossRef] [PubMed] [Google Scholar]
- The Tobacco Products (Prohibition of Advertisement and Regulation) Bill. 2001. Globalink; Available from: http://www.globalink.org/tobacco/docs/ap-docs/legislation/0103aghi [Last accessed on 2022 Jun 17]
- [Google Scholar]
- GATS 2 Fact Sheet India. 2016-17. Available from: https://tiss.edu/uploads/files/National_FactsheeIndia.pdf [Last accessed on 2022 Jun 17]
- [Google Scholar]
- World Health Organisation Tobacco Free Initiatives/ MPOWER. Available from: https://www.who.int/initiatives/mpower [Last accessed on 2022 Jun 17]
- [Google Scholar]
- Strategies for tobacco control in India: A systematic review. PLoS One. 2015;10:e0122610.
- [CrossRef] [PubMed] [Google Scholar]
- Resource Center for Tobacco Control; Policies and legislations. Available from: https://www.rctcpgi.org/index.php [Last accessed on 2022 Jul 20]
- [Google Scholar]
- Initiating tobacco cessation services in India: Challenges and opportunities. WHO South East Asia J Public Health. 2012;1:159-68.
- [CrossRef] [PubMed] [Google Scholar]
- Tobacco cessation in India: A priority health intervention. Indian J Med Res. 2014;139:484-6.
- [Google Scholar]
- Establishment of Tobacco Cessation Centres in Dental Institutes an Integrated Approach In India: Operational Guidelines. 2018. Available from: https://dciindia.gov.in/Rule_Regulation/FinaloperationalguidelinesTCCindentalcolleges.pdf [Last accessed on 2022 Jun 17]
- [Google Scholar]
- The effect of a clinic-based behavioral intervention in promoting enrolment in a text-message tobacco cessation program at a rural primary health clinic in Delhi, India. Tob Prev Cessat. 2020;6:27.
- [CrossRef] [PubMed] [Google Scholar]
- Government of India mCessation Programme Quit Tobacco for Life. Available from: https://www.nhp.gov.in/quit-tobacco-about-programme_mtl [Last accessed on 2016 Dec 23]
- [Google Scholar]
- Tobacco Quitline. Available from: https://iasgatewayy.com/tobacco-quitline [Last accessed on 2022 Jun 17]
- [Google Scholar]







