Translate this page into:
Barriers to access dental care services among adult population: A systematic review

*Corresponding author: Dr. Lakshmi Krishnan, SH109, ECR, Uthandi, Tamil Nadu-119, India. lakshmi.krish24@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Krishnan L, Aarthy CS, Kumar PD. Barriers to access dental care services among adult population: A systematic review. J Global Oral Health 2020;3(1):54-62.
Abstract
Objective:
This systematic review was done with the aim of assessing the barriers faced in utilizing dental care services by general population in age group between 20 and 60 years in India as these findings would provide evidence for making appropriate decisions in our National Oral Health Policy which could further improve access to dental care services for people across India. This was a systematic review.
Materials and Methods:
For this review, PubMed, TRIP database, Cochrane, and Google Scholar were the electronic databases searched based on the PICO. Preferred Reporting Items for Systematic Reviews and Meta- Analyses guidelines were followed for the final inclusion of articles.
Results:
The search generated a total of 91 articles from four different electronic bases: PubMed, TRIP database, Cochrane, and Google Scholar. Based on the inclusion criteria, 14 articles made it to the final analysis. All 14 studies reported a lack of time and nonavailability of dentists as major barriers in accessing dental care services.
Conclusion:
The cross-sectional studies of this review were assessed for quality using a modified Newcastle- Ottawa Scale, proposed by Egger et al. in 2003. Even though the available literature forms a lower standard of evidence, further evaluation of barriers using a standardized questionnaire is recommended using better-designed studies to substantiate the unequal access to health-care facilities to Indian Population.
Keywords
Indian population
Barriers
Utilization
Dental services
INTRODUCTION
The oral health of the general population in various countries across the globe has shown an improved trend over the past few decades, but people from developing countries still continue to have profoundly high levels of dental disease mainly dental caries and periodontal disease.[1] Literature evidences show that suboptimal utilization of dental care services has been repeatedly reported by the population from developing countries.[2,3] In many countries, comprehensive national dental care systems have succeeded in increasing the coverage and reducing or even eliminating socio-economic differences in the use of dental services.[4] However, inequalities in socioeconomic status lead to uneven utilization of dental services in many countries. There are also other barriers to seeking regular dental care, including the availability of dental services, dental fear, cost, income the distance a person had to travel to get care, and preference for preservation of teeth. The Federation Dentaire Internationale classifies barriers for utilizing dental services as follows: (a) Individuals themselves (such as lack of perceived need, anxiety or fear, financial considerations, and lack of access), (b) the dental profession (inappropriate workforce resources, uneven geographical distribution, training inappropriate to changing needs and demands. and insufficient sensitivity to patient’s attitudes and needs), and (c) society (insufficient public support of attitudes conducive to health, inadequate oral health care facilities, inadequate oral health workforce planning, and insufficient support for research).[5-7] Utilization is the actual attendance by the members of the public at health-care facilities to receive care. Utilization, which measures the number of visits per year or the number of people with at least one visit during the previous year, serves as an important tool for oral health policy decision-making.[8] The primary purpose of dental care services is to provide good dental health. An improvement in the individual level of dental health is an important indicator of the overall performance of the communities’ dental care system. Thus, a change in individual dental health will have an impact on the demand as well as the utilization of dental services across the communities and finally the nation.[9]
India being one of the largest democracies in the world, with a population of over 1 billion is a rapidly developing nation and is making great progress in IT, finance, and living standard. In spite of these, it is alarming to know that very few people receive proper and good dental care. This could be substantiated by the fact that about a third of the population suffer from dental caries that require treatment.[10]
Over the years, the Government of India has shown an increase of 16% in the allocation of monetary resources to the health sector from 2018 to 2019.[11] Despite this rise, the budget allotted to oral care is very minimal. Furthermore, there are no preventive care policies and recall systems for regular checkups and the dental care provided is treatment-oriented. In our country, dental care services are mostly through out of pocket expenses by the patient, with very limited influence of private/public insurance companies. Therefore, finance becomes a huge barrier to access dental care.[12,13]
Another problem encountered by the patients in accessing dental care can be attributed to diversity in the distribution of dental care providers. Previous studies have shown the inappropriate distribution of workforce with states in Southern and Eastern region harboring thousands of dentists whereas northeastern and northwestern regions lack adequate workforce.[14]
Apart from all these disparities, India is also a country with great cultural diversity; its influence contributes and plays an integral part in shaping and developing good oral hygiene practice. In many cultures, the esthetic appearance of teeth may be important, but having “healthy” teeth and gums is not related to the appearance in a direct way. Health care is a cultural construct arising from beliefs about the nature of the disease and the human body, and it follows that cultural issues are a hindrance to the delivery of effective preventive care and illness intervention.[13]
To address these problems, various bodies including Indian Dental Association, Dental Council of India work toward equitable access to oral care by conducting camps for various populations around the country, distribution of oral hygiene kits, training personnel to conduct a basic oral examination, and targeting school children through school dental programs. Despite such tremendous efforts taken by these bodies, our country still faces a huge oral disease burden. As an initiative to rectify the situation, the Ministry of Family Health and Welfare came up with national oral health policy in 1986. This policy was formulated along with National Oral health Programme to address the issues of:
Determinants to improve oral health
Integration of oral health promotion and preventive services with the general health-care system
Promoting of public-private partnerships (PPP) model for achieving better oral health.[15]
Further to alleviate the problem, Ayushman Bharat or “Healthy India” is a national initiative launched by Prime Minister Narendra Modi as the part of National Health Policy 2017, to attain the goal of Universal Health Coverage. This program has been sketched in a manner to achieve SDG goals and its underlying principle which says “leaving no one behind.” Ayushman Bharat is an initiative to make headway from a segmented outlook of health- care delivery to a comprehensive need-based health-care service. Its functions focus mainly on delivering treatments, which address health in a holistic approach (covering prevention, promotion, and ambulatory care) covering all levels of prevention. This scheme will be in action through Health and Wellness Centres within the primary health center or sub-center in the village and that will be providing preventive, promotive, and curative care for non- communicable diseases, psychiatric care, geriatric care, and palliative care along with dental care.[16] Unfortunately, all these proposals are still in a draft stage. Although it is evident that dental care access in our country encounters numerous barriers, majority of them are not rectified. A first step to any problem will be an in-depth understanding of the same, which when carried out by systematically analyzing the available literature forms the highest scientific evidence. Thus, this systematic review was done with the aim of assessing the barriers faced in utilizing dental care services by general population in age group between 20 and 60 years in India as these findings would provide evidence for making appropriate decisions in our national oral health policy which could further improve access to dental care services for people across India.
MATERIALS AND METHODS
Design
A systematic review was undertaken using objective and transparent methods as per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines to identify, evaluate, and summarize all relevant research findings. The protocol for this review is submitted to PROSPERO and the final number is yet to be assigned by the concerned body [Registered number-130431].
Eligibility criteria
On applying the PICO analysis to the articles searched the criteria were set as shown below:
-
PICO Analysis
Population – Indian adults in the age group of 20–60 years
Interest – Barriers to utilize dental care services
Comparison – Not applicable
Outcome – Barriers encountered while accessing/ utilizing dental care services.
Since the research question for this review is qualitative in nature in PICO analysis instead of “intervention” “Interest” was used, and “Comparator” was not applicable.
Inclusion criteria
Studies assessing the barriers to dental care service utilization in India among adults as their primary objective
Studies which had defined dental care utilization as the proportion of population who access dental services over a specified period of time
The search included only studies published in English
The review focused on studies which reported the patient’s perception of barriers to dental care services in India
Studies which had a population in the age range between 20 and 60 years
Studies published in the past 10 years were included
Studies with cross-sectional and cohort designs were considered.
Exclusion criteria
Studies reporting dentist perception on barriers to dental care utilization among the adult population in India
Studies reported on barriers to dental care utilization among the population with special needs
Narrative reviews, expert opinion, and case studies
Publications with no abstract and those which were widely out of the scope of the study were eliminated
Studies required translation to the English language.
The remaining studies were sorted on the basis of their title and abstract. Finally, those studies in which the abstract fulfill all inclusion criteria were selected for full-text reading. In those cases in which a study met the eligibility criteria but the information in the abstract was insufficient, full texts of the articles were also obtained. Further literature search was performed based on the bibliography of the selected articles.
Search strategy
Relevant studies were included from the period of January 2008 to December 2018 through MEDLINE (PubMed), Cochrane, TRIP, and Google Scholar. A detailed search strategy was developed for MEDLINE through the use of MeSH terms and was revised for TRIP, Google Scholar, and Cochrane. The first set of terms includes “barrier to dental service” and “oral health care” separated by Boolean operator OR. The second set included the term “access,” and “utilization” separated by Boolean operator “OR” and the third set included the term “Indian adults,” and “adult population” “India” separated by Boolean operator “OR.” Data searches were done during the time period of December 2018 and again in March 2019 by two authors (LK and MK) independently. Hand searches of reference lists of included studies were conducted to ensure additional relevant references were identified. Although systematic reviews, narrative reviews were excluded, reference lists were checked to ensure all primary research was located for inclusion. Only full papers written in English were included. Where multiple publications reporting on the same study existed in different databases, data from the study were extracted and reviewed only once. Duplication of the article was identified using RevMan software (Version 5.3).
Table 1 depicts the search applied in terms of MeSH terms and search words for each database
| Database | Search pattern |
|---|---|
| PubMed | (((barriers[All Fields] AND ((“utilization” AND (“dental care”[MeSH Terms] OR (“dental”[All Fields] AND “care”[All Fields]) OR “dental care”[All Fields] OR “dental services”[All Fields]))) AND “India”[All Fields]) OR “indian adult”[All Fields])) OR ((“adult population”[MeSH terms]OR “adults”[All Fields])) |
| Cochrane |
IDSearch #1-MeSH descriptor: dental care services #2-Barriers #3-MeSH descriptor: India #4-adult population #5-adult or adults #6- #1 and #2 #7-#3 and #4 #8-#5 and #6 and #7 |
| Google Scholar and TRIP | “Barriers to dental care services” “oral health care” “ access” “Indian adult population” |
Study selection
Study selection was conducted by two authors (1st and2nd authors) who independently screened titles and abstracts against the inclusion/exclusion criteria and identified relevant papers. Then, the same two authors independently reviewed the full-text studies which they were unable to be excluded by title and abstract alone. A comparison of papers was completed between the two authors with no disagreements regarding inclusion. The final articles selected were then cross verified by the 3rd author. The inter-rater agreement was found to be 0.8.
Data extraction
The data extraction from the final 16 articles was done using a data extraction form. It includes the first author name, year of publication of the article, study population, objectives of the study, study design, method of obtaining relevant information (Assessment Tool), results of primary outcome, and author’s conclusion.
Quality assessment of the included studies
The final analysis included 14 cross-sectional studies and the methodological quality of the selected articles was assessed using the modified Newcastle-Ottawa Scale. For cross-sectional studies, the quality score was based on five items of the following categories: Group selection, outcome, and exposure. A maximum score of five points for group selection and exposure and three points for outcome were recorded to determine the methodological quality of the included studies. The higher the score, better the quality of the study.
Since there is no evident tool to assess the risk of bias for cross-sectional studies, based on our review objective, sample representativeness and assessment tool used were criteria chosen to determine the risk of bias across studies.[17]
RESULTS
Search results
The search generated a total of 91 articles from five different electronic bases: PubMed, TRIP, Cochrane, and Google Scholar. PubMed produced 17 articles, TRIP database produced six articles, Cochrane produced nine articles, and Google Scholar produced 54 articles. PRISMA 2009 guidelines regarding the paper selection are shown as a flowchart in Figure 1.
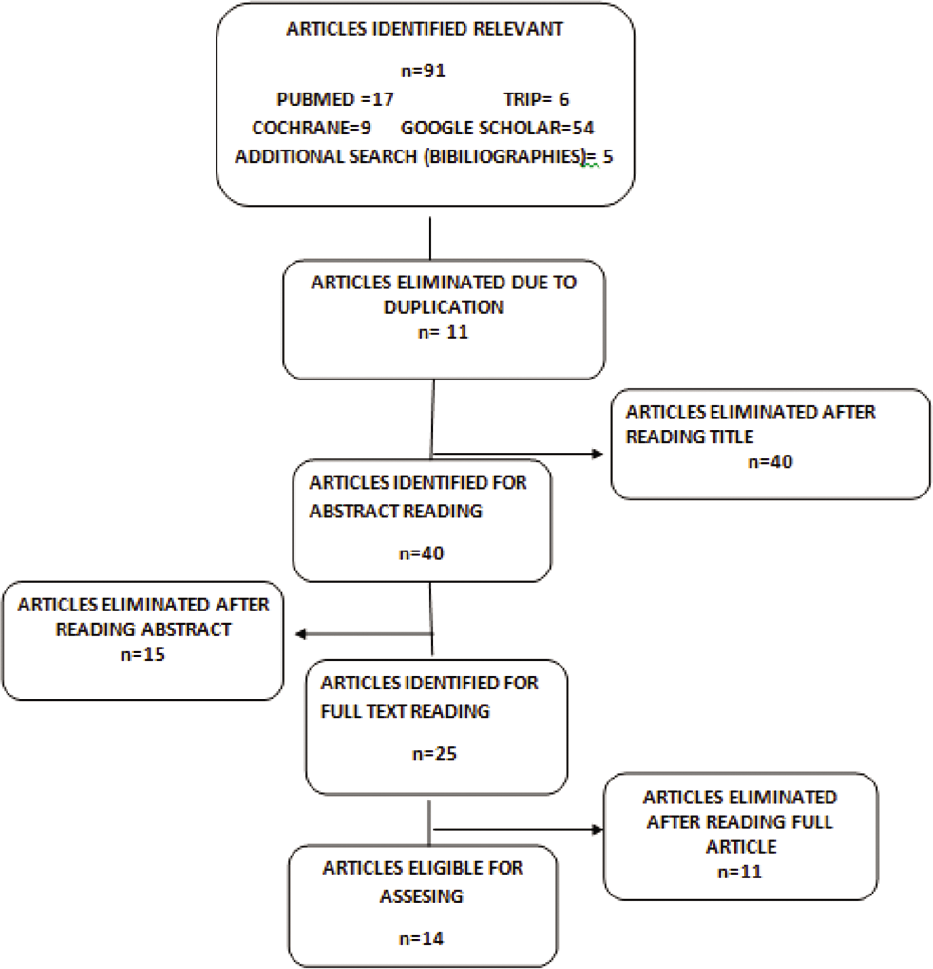
- The search strategy according to the PRISMA guidelines.
Figure 1 shows the search strategy according to the PRISMA guidelines.
The full texts of 25 articles were obtained for further review. On the basis of inclusion and exclusion criteria, nine articles were included initially in this systematic review. The bibliographical search of the selected articles yielded an additional five eligible studies for inclusion. Hence, a total of 14 articles were considered for the final review. Among those 11 articles excluded, seven articles had reported barriers reported by geriatric patients and pediatric patients. Four articles had a study population of dentists reporting on barriers encountered by them in delivering dental care services. All the studies included were cross-sectional design.
The methodological quality and risk of bias were assessed using the Modified Newcastle-Ottawa Scale. Among the 14 articles included, four articles had a moderate methodological quality and a higher risk of bias when compared to the rest ten articles which had less risk of bias and good quality of methodology. Figure 2 shows the quality assessment along with the risk of bias across the 14 articles included.

- Representing the methodological assessment of the 14 included articles.
Figure 2 represents the methodological assessment of the 14 included articles.
The author’s name with year of publication, study population, assessment tool, outcome, and summary of these included studies are tabulated in Table 2.
| S. No. | Author and Year | Population | Outcome and Result | Author’s conclusion |
|---|---|---|---|---|
| 1. | Poudyal et al., 2010[19] |
n=195 adults Age group-above 18 years |
No issues in teeth – 60.7% Lack of time – 12.7% Fear – 12% Not a priority – 4.7% Long distance – 1.3% No knowledge – 5.3% |
Majority reported “I have not had any problems in my teeth” as reason for not visiting a dentist |
| 2. | Kakatkar et al., 2011[35] |
n=427 Age group 25–45 years |
Lack of knowledge – 11.7% No time – 27.4% No interest – 33.3% Difficulty in getting appointment – 23.2% Unpleasant experience – 41. l% Costly – 20.4% Transportation difficult – 21.3% Work restraint – 14.3% Lazy – 4% Not a priority – 19.4% |
The highly reported reason for not visiting a dentist in this study was “fear toward the dentist” |
| 3. | Randhawa et al., 2011[21] |
n=1232 Age group 30–60 years |
No time – 32.14% Local medicine usage – 30.6% Transportation difficulty – 36.86% |
Uneven distribution of dentist ratio in urban and rural areas were the reason for nonutilization |
| 4. | Kadaralu et al., 2011[24] |
n=246 adults Age 18–55 years |
Expensive – 22% Time constraint – 19.5% Fear – 8.5% Lack of transportation – 1.2% Other reasons – 2.4% |
High cost was the main barrier to the utilization of dental services |
| 5. | Devaraj et al., 2012[27] |
n=180 people Age 15–65 years |
Not a priority – (43.1%) Neglect – (22.4%) No teeth problems – (15.5%) Time constraint – (8.6%) Costly – (6.9%) Fear of dentist – (1.7%) More visits – (1.7%) |
Majority did not prioritize oral health |
| 6. | Verma et al., 2012[22] | n=193 | Not important – (45%) No time – (22%) Usage of self-medicines – (16%) |
This study has revealed the gaps in the knowledge of the respondents, about dental problems as a barrier |
| 7. | Fotedar et al., 2013[18] |
n=319 adults Age group – above 18 years |
No time – 39.3% Expensive – 10.6% Not needed unless has pain – 62.5% Fear – 31.5% Long distance – 49.3% not a priority – 61.8% |
Majority reported barrier for visiting a dentist was “Not needed unless has pain” indicating the low felt need of the people |
| 8. | Jain et al., 2013[36] |
n=600 Age group – 20–50 years |
No issues in teeth – 25% Lack of knowledge – 65% Not a priority – 78% No interest – 14.5% Unpleasant experience – 24.5% Lack of time – 20.25% Fear – 60.3% Costly – 74% No dentist nearby – 75.3% Traveling to the dentist is too difficult – 72% Lack of adequate transport to dental care facility – 56% Time restraint – 23.6% Lazy – 10.7% |
Highly reported barriers for utilization of oral health care were: Knowledge, attitude, fear, cost, and transport |
| 9. | Gill et al., 2014[20] |
n=400 Age group-older than 20 years |
Lack of time – 190 Not a priority – 115 Usage of local medicines – 95 |
Lack of time was identified as the major barrier in this study |
| 10. | Nagarjuna et al., 2016[25] |
n=600 Age group-older than 20 years |
Lack of time – (45.8) Costly – (33.3) Not a priority – (60) Fear – (48.6) Long-distance – (26.3) I do not think dental diseases are very serious – (51) |
Most of them believe that visiting the dentist is necessary only for pain relief |
| 11. | Patel et al., 2016[23] |
n=450 Age group 18–60 years |
Lack of knowledge6.5% More visits –35% Expensive – 61.5% |
Myths and beliefs create hindrances in the effective delivery of quality preventive and corrective dental treatment |
| 12. | Fozia et al., 2017[28] |
n=120 Age 20–67 years |
No issues in teeth – 46.4% (Beliefs and Myths) –8.6% Financial difficulty –6.4% Lack of time – 27.6% Anxiety and fear of dental treatment – 6.9% Transportation – 4.1% |
The highly reported reasons for nonutilization of dental service in this study were “Did not have any dental problem” |
| 13. | Francis et al., 2017[29] |
n=420 Age 20–67 years |
Did not have any dental problem – 46.4% The dental problem was not serious – 8.6% Financial difficulty – 6.4% Lack of time – 27.6% Anxiety and fear of dental treatment – 6.9% Transportation – 4.1% |
The highly reported reasons for nonutilization of dental service in this study were “Did not have any dental problem” indicating the low felt need among study subjects in that area |
| 14. | Vashisht et al., 2018[26] |
n=545 Age group – 18–44 years |
Financial constraints (42.0%) Lack of transportation facility (23.7%) Nonavailability of dentist (6.1%) Lack of time (79.4%) Lack of symptoms (82.4%) Anxiety toward dental procedures (64.1%) |
Majority reported a lack of tooth symptoms as the reason for not visiting the dentist |
Main findings
All the included studies reported barriers faced by the adult population aged 20–60 years in utilizing dental health services in India.
Assessment tool
All the 14 studies have used a self-administered structured questionnaire to assess the barriers faced by the adult population in utilizing dental care services; in India. These structured questionnaires had questions related to socio-demographic characteristics, barriers faced in utilizing dental services were reported in the included studies and five studies Fotedar et al.,[18] Poudyal et al.,[19] Gill et al.,[20] Randhawa et al.,[21] and Verma et al.[22] had added questions on attitude and practice toward oral hygiene measures, oral health status of these population was also recorded. One article by Patel et al.[23] focused mainly on cultural and socio-economic status as barriers to dental service utilization. Another study by Kadaluru et al.[24] assessed the self-perception of oral health of the population. All these studies made a descriptive analysis of the questionnaire which was validated in a similar population before being used as a tool to assess the barriers to dental service utilization among children with special needs.
Study population
Included studies had a sample size ranging between 120 and 1200 adult population. Age of the study population was defined in most of the included except in five studies – Nagarjuna et al.,[25] Gill et al.,[20] Poudyal et al.,[19] and Fotedar et al.,[18] where the upper limit of age was not defined, whereas in study done by Verma et al.,[22] the age of the population was not defined at al.
Oral health status
Among the studies which were analyzed, studies had analyzed the oral health status of the population. In the study conducted by Poudyal et al.,[19] the majority of the participants had tooth decay (42%), whereas Verma et al.[22] presented tooth decay to be 93% in his study. In another study conducted by Randhawa et al.,[21] he reported the prevalence of oromucosal lesions as 9.7%, dental caries as 59.6%, periodontal disease as 52.8%, 34.3%-fluorosis, and around 43.3% as edentulous.
Dental care service utilization rate
Vashisth and Gupta[26] in his study reported that 24% of the adult population had never visited a dentist. Devraj and Eshwar[27] states that 38.3% of the adult population had last utilized the services before 2 years, whereas in the study conducted by Fotedar et al.[18] it was 52% of the population. Poudyal et al.[19] in her study points out that 46% of the patients had not visited the dentist so far for their tooth problems which were similar to the study conducted by Gill et al.[20] who reported 60%. In the study conducted by Verma et al.[22] reported 26% of non-attendance to dental services and 33.3% of non-attendance was reported by Randhawa et al.[21] In another study done by Kadaralu et al.,[24] 33.1% of participants visit the dentist once a year.
Out of the 14 studies analyzed, seven studies done by Randhawa et al.,[21] Kadaralu et al.,[24] Verma et al.,[22] Poudyal et al.,[19] Devraj and Eshwar, Fotedar et al.,[18] and Vashisth and Gupta[26] reported the percentage of population utilization of dental care services pattern.
Barriers to dental care services – through caregiver’s perception
The most common barriers encountered by the adult population in India as reported by all the 14 studies, include “lack of time and “transportation difficulty/Nonavailability of dentist.” Another common barrier perceived by the population was “fear/anxiety of dental procedures due to previous experiences “which was seen among eight studies. Finance was seen as a constraint in studies conducted by Kadaralu et al.,[24] Foterdar et al.,[18] Fozia et al.,[28] Francis et al.,[29] and Vashist and Gupta.[26] Lack of knowledge on oral health care/considering dental problems less serious was seen to be a significant barrier among the adult population which was reported among eight studies included.
DISCUSSION
The intent of this systematic review was to find the barriers faced by the Indian adult population within the age group of 20–60 years; through self-reported questionnaires. Population in the age group below 18 years and above 60 years were excluded as utilization of health services in both these populations are influenced by various other factors such as parental/caregivers perception, comorbid health condition or physical difficulty to access health services.[30] The search was restricted to India because in recent years, there has been tremendous change in oral health patterns among the population, and the National Oral Health Policy has reached its second draft stage. With a deeper understanding of the barriers faced in utilizing dental services through systematically analyzing literature would prove to be a platform for the stakeholders to modify/ devise appropriate policies across the country. Despite the high number of publications in this field that was initially screened, the relatively small number of studies that were finally included in the review collaborates the idea that there is a lack of quality evidence on barriers faced by the Indian adult population in utilizing dental care services.
In the present review, the search based on PRISMA guidelines narrowed down on a set of 14 descriptive cross-sectional studies that reported an outcome on barriers faced in utilizing dental care services by the Indian adult population between 20 and 60 years of age.
Over the years, the pattern of oral health status has improved across the globe yet India faces increased dental disease burden among its residents.[1] The reason could be due to inequalities seen in accessing dental services and poor planning and implementation of health programs. Despite numerous health schemes cropping up the surfaces, oral health still occupies a back seat. An increased unmet dental need was seen among the studies participants of the included studies with decrease in utilization pattern of oral health services.[10]
Among the 14 included studies, seven studies had reported utilization rate of dental services among the participants, which showed a greater variation. A higher rate of nonutilization was seen among the northeastern states which could be attributed to the uneven distribution of dentists. In accordance to the above statement, all the included studies reported nonavailability of dentist as a major barrier in accessing dental services.[21] Reasons for higher utilization rate and anticipated reason for nonutilization of dental services could be the socio-economic status of the subjects; the perception of the adult about dental service is some of the significant predictive factors of dental service utilization. Patel et al. in their study showed a significant association in income, racial ethnicity, and education with unmet needs of dental care.[23]
Apart from these, there are also other barriers in seeking regular dental care, including dental fear, finance, lack of knowledge/time, and less importance given to the oral disease. In our systematic review, the above-mentioned barriers were the most common ones reported.
Patients’ feelings, beliefs, and attitude are some of the psycho- social determinants of dental health which modify or change the patient’s dental health-care seeking behavior but may prove to be the basis for the barriers in accessing dental health care.[31] Several literature studies state inadequate dentist workforce distribution, poor knowledge, lack of insurance schemes for dental care, poor government policies, and fear toward dentists as potential barriers for their access to oral care, which is very well reflected in this review.[32-36] Although dental care delivery is a two-way process, the receiving end always has an upper hand whose feedback plays a pivot role in a system. Therefore, all the articles selected for analysis had the patient’s perceptions of barriers faced in dental care service utilization as their primary outcome. Overall findings of this study suggest that the utilization of dental services among the Indian adult population shows huge variation and there are barriers at individual, interpersonal, environmental, and governmental level factors which act as barriers in accessing and utilization of dental care services. From the current literature evidence, we can conclude the geographic imbalance of dentists, lack of knowledge and time, financial constraint as profound barriers present in dental service utilization among the Indian adult population.
Limitations
Certain limitations can be noticed in the search criteria and study design. The search included studies reporting barriers faced by patients alone, because of these four studies were excluded that may have provided additional evidence. Furthermore, the questionnaires used in all the included studies were not standardized, hence reporting bias would influence the final result of the review. It was not possible to synthesize the data using statistical analyses given the heterogeneity and lower level of evidence within the included studies.
CONCLUSION
The lack of high-quality evidence about the barriers faced by the adult population in India will remain a challenge to many dental clinicians as the gap created between unmet dental needs and utilization of dental services still remain unbridged. Although various barriers are listed, lack of time and unavailability of the dentist seems to be more common ones faced. Henceforth, for further evaluation of the barriers to utilization of dental care services among the Indian adult population, a standardized questionnaire tool would improvise the standards of the studies in the future.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- India State-Level Disease Burden Initiative Collaborators. Nations within a nation: Variations in epidemiological transition across the states of India, 1990-2016 in the global burden of disease study. Lancet. 2017;390:2437-60.
- [Google Scholar]
- Oral Health Inequalities and Health Systems in AsiaPacific. Nature India Annual Issues.
- [Google Scholar]
- Global, regional, and national prevalence, incidence, and disability-adjusted life years for oral conditions for 195 countries, 1990-2015: A systematic analysis for the global burden of diseases, injuries, and risk factors. J Dent Res. 2017;96:380-7.
- [CrossRef] [PubMed] [Google Scholar]
- Global, regional and country-level economic impacts of dental diseases in 2015. J Dent Res. 2018;97:501-7.
- [CrossRef] [PubMed] [Google Scholar]
- The health system in India: The underserved majority. Lancet. 2017;390:2426-7.
- [CrossRef] [Google Scholar]
- Underutilization of dental care when it is freely available: A prospective study of the New England children's amalgam trial. J Public Health Dent. 2008;68:139-48.
- [CrossRef] [PubMed] [Google Scholar]
- Factors influencing use of dental services in rural and urban communities: Considerations for practitioners in underserved areas. J Dent Educ. 2004;68:1081-9.
- [CrossRef] [PubMed] [Google Scholar]
- Use of dental services: An analysis of visits, procedures and providers, 1996. J Am Dent Assoc. 2002;133:167-75.
- [CrossRef] [PubMed] [Google Scholar]
- The concept of access: Definition and relationship to consumer satisfaction. Med Care. 1981;19:127-40.
- [CrossRef] [PubMed] [Google Scholar]
- Burden of dental diseases in India as compared to South Asia: An insight. Indian J Dent Res. 2018;29:374-7.
- [CrossRef] [PubMed] [Google Scholar]
- GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: A systematic analysis for the global burden of disease study 2016. Lancet. 2017;390:1211-59.
- [CrossRef] [Google Scholar]
- Is the utilisation of dental care based on need or socioeconomic status? A study of dental care in Indonesia from 1999 to 2009. Int Dent J. 2012;62:90-4.
- [CrossRef] [PubMed] [Google Scholar]
- Socioeconomic inequalities in dental services utilisation in a Norwegian county: The third Nord-Trondelag health survey. Scand J Public Health. 2012;40:648-55.
- [CrossRef] [PubMed] [Google Scholar]
- Addressing inequalities in oral health in India: Need for skill mix in the dental workforce. J Family Med Prim Care. 2015;4:200-2.
- [CrossRef] [PubMed] [Google Scholar]
- Operational Guidelines National Oral Health Program Ministry of Health and Family Welfare Government of National Oral Health Cell Directorate General of Health Services Ministry of Health and Family Welfare Government of India. 2012-2017
- [Google Scholar]
- How to critically appraise an article. Nat Clin Pract Gastroenterol Hepatol. 2009;6:82-91.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers to the utilization of dental services in Shimla, India. Eur J Gen Dent. 2013;2:39-43.
- [CrossRef] [Google Scholar]
- Utilization of dental services in a field practice area in Mangalore, Karnataka. Indian J Community Med. 2010;35:424-5.
- [CrossRef] [PubMed] [Google Scholar]
- Oral hygiene practices, attitude, and access barriers to oral health among patients visiting a rural dental college in North India. J Dent Res Rev. 2014;1:114-7.
- [Google Scholar]
- Assessment of oral health status, treatment needs, coverage and access barriers of patients reporting to a rural dental college in Northern India. J Indian Assoc Public Health Dent. 2011;18:899-904.
- [Google Scholar]
- Access to public dental care facilities in Chandigarh. Indian J Dent Res. 2012;23:121.
- [CrossRef] [PubMed] [Google Scholar]
- Cultural and socioeconomic barriers in utilization of dental services: A cross sectional questionnaire based study. Natl J Community Med. 2016;10:807-10.
- [Google Scholar]
- Utilization of oral health care services among adults attending community outreach programs. Indian J Dent Res. 2012;23:841-2.
- [CrossRef] [PubMed] [Google Scholar]
- Utilization of dental health-care services and its barriers among the patients visiting community health centers in Nellore district, Andhra Pradesh: A cross-sectional, questionnaire study. J Indian Assoc Public Health Dent. 2016;14:451-5.
- [CrossRef] [Google Scholar]
- Barriers to utilization of dental care services in rural area of Panchkula district, Haryana, India. Int J Sci Res. 2018;7:62-3.
- [Google Scholar]
- Reasons for use and non-use of dental services among people visiting a dental college hospital in India: A descriptive cross sectional study. Eur J Dent. 2016;6:422-7.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers in utilization of dental services among Kashmiri population a cross sectional study. Int J Appl Dent Sci. 2017;3:416-8.
- [Google Scholar]
- Barriers in utilization of dental services among Chennai population, Tamil Nadu, India a cross sectional survey. Eur J Pharm Med Res. 2017;4:667-70.
- [Google Scholar]
- Barriers to the provision of comprehensive dental care in geriatric patients. Indian J Med Res Pharm Sci. 2017;4:8-12.
- [CrossRef] [Google Scholar]
- Barriers to dental care utilization in India. J Indian Assoc Public Health dent. 2011;7:721-3.
- [Google Scholar]
- Barriers to accessing and accepting dental care. Br Dent J. 1999;187:81-4.
- [CrossRef] [Google Scholar]
- Access to oral health care in India: Overview. Unique J Med Dent Sci. 2015;3:56-60.
- [Google Scholar]
- Utilization of dental care: An Indian outlook. J Nat Sci Biol Med. 2013;4:292-7.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers to the utilization of dental services in Udaipur, India. J Dent (Tehran). 2011;8:81-9.
- [Google Scholar]
- Barriers in utilization of oral health care services among patients attending primary and community health centres in Virajpet, South Karnataka. Natl J Med Dent Res. 2013;1:39-47.
- [Google Scholar]






