Prevalence of developmental defects of enamel among children with intellectual disability – A systematic review

*Corresponding author: C. S. Aarthy, Department of Public Health Dentistry, Ragas Dental College and Hospital, Chennai - 600119, Tamil Nadu, India. aarthycharms@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Aarthy CS, Kumar PD. Prevalence of developmental defects of enamel among children with intellectual disability – A systematic review. J Global Oral Health 2020;3(1):49-53.
Abstract
The purpose of this review was formulated with an aim to understand the prevalence of enamel defects among ID children. An identical search was performed in PubMed, Google scholar, and Cochrane review and was limited to human studies and studies written in English. Reviews, case studies, and case series were excluded from the study. A total of 56 articles were identified. In PubMed 18 articles, Google scholar 29 articles and Cochrane review nine articles were found, respectively. In this, two studies (n = 2), dealt with the developmental defects of enamel with intellectual disability (ID)/mental retardation. This systematic review suggests that developmental defects of enamel was more common in ID children than normal children. A larger number of well designed studies are, however, needed to increase the validity of the studies.
Keywords
Intellectual disability
Developmental defects of enamel
Enamel hypoplasia
Germ layer
INTRODUCTION
A germ layer is a primary layer of cells that forms during embryonic development. Germ layers eventually give rise to all of the tissues and organs through the process of organogenesis. Germ layers are endoderm, mesoderm, ectoderm, and neural crest. Ectoderm is the outer layer of the embryo, and it forms from the embryo’s epiblast. It develops into the surface ectoderm, neural crest, and neural tube. Surface ectoderm develops into epidermis, hair, nails, lens of the eye, and tooth enamel. The neural crest of the ectoderm develops into peripheral nervous system, adrenal medulla, and dentin of teeth. The neural tube of the ectoderm develops into brain, spinal cord, motor neurons, and retina.[1] If any defects occurs in the formation of ectoderm derivatives, its effects will be evident in the respective organs developed from the germ layer. This could be explained by the fact that all these organs develop from the same germ layer. One such defect could be intellectual disability (ID) and enamel defect.
ID is defined as a group of developmental conditions characterized by significant impairment of cognitive functions which are associated with limitations of learning, adaptive behavior, and skills.[2] Overall, In India, the prevalence of ID is 10.5/1000 with urban population having slightly higher rate (11/1000) than rural (10.08/1000) population.[3]
Literature search reveals that the risk factors of intellectual disabilities are prenatal, perinatal, and postnatal. The prenatal factors strongly associated with ID risk are advanced maternal age, maternal alcohol use, and maternal epilepsy. Other significant factors with a lower strength of association are maternal tobacco use, maternal diabetes, and maternal asthma.[4] Literature evidence states that maternal health is strongly associated with brain development of the fetus.[5] Some studies state that enamel hypoplasia is more common in children with cerebral palsy, intellectual disabilities, or hearing defects, which suggests that certain systemic disruptions interfering with neurological development may also alter the development of tooth germ. Damaged enamel cannot recover from the injury; therefore, it may give information on the timing and nature of insults potentially affecting other ectodermally derived structures, such as the brain.[6] Hence, enamel defects can be used as predictive risk factors for intellectually disabled children.
This systematic review was formulated with an aim to understand the prevalence of enamel defects among ID children. The results of this review would help policy makers and stake holders of country to provide better dental preventive program for these children as enamel defects pose a profound threat to develop dental caries.
MATERIALS AND METHODS
Design
A systematic review was undertaken using objective and transparent methods as per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, to identify, evaluate, and summarize all relevant research findings.
Eligibility criteria
On applying the PICO analysis to the articles searched, the criteria were set as shown below:
-
PECO analysis
Population - Children with ID
Exposure – ID
Comparison - Children without any disabilities
Outcome - Developmental defects of Enamel.
Inclusion criteria
Studies which assessed the developmental defects of enamel among ID using the Modified Developmental Defects of Enamel (MDDE) index were included in the study.
Studies which had a sample of children within the age group of 5–18 years were included in the study.
Studies which had assessed the developmental defects of enamel as a primary and secondary objective were included in the study.
Cross-sectional studies were included in the study.
The search included only studies published in English.
Studies published in the past 8 years were included in the study.
Exclusion criteria
The following criteria were excluded from the study:
Studies which assessed the developmental defects of enamel using indices other than modified developmental defects index were excluded.
Studies which assessed the combination of disabilities were excluded.
Qualitative studies, reviews, expertz opinion, systematic reviews, meta-analysis and case studies/series.
Publications with no abstract and those which were widely out of scope of the study were eliminated.
Studies that required translation to English language.
The remaining studies were sorted on basis of their title and abstract. Finally, those studies in which the abstract fulfill all inclusion criteria were selected for full-text reading. In those cases, in which a study met the eligibility criteria but the information in the abstract was insufficient, full texts of the articles were also obtained. Further literature search was performed based on the bibliography of the selected articles.
Search strategy
Relevant studies were included from the period of June 2011– December 2018 through MEDLINE (PUBMED, GOOGLE SCHOLAR, and COCHRANE REVIEW. A detailed search strategy was developed for MEDLINE through the use of MeSH terms and was revised for Google Scholar also. The first set of terms include “Intellectual disability,” “Enamel hypoplasia” separated by Boolean operator OR. The second set included the term “children with intellectual disability,” “Developmental defects of enamel” separated by Boolean operator “AND” “and the third set included the term “Prevalence and Intellectual disability,” separated by Boolean operator “AND. Data searches were done at December 2018. Hand searches of reference lists of included studies were conducted to ensure additional relevant references were identified. Although systematic reviews, qualitative studies were excluded. Only full papers written in English were included. Where multiple publications reporting on the same study existed in different databases, data from the study were extracted and reviewed only once. Duplication of article was identified using software.
Study selection
Study selection was conducted by two authors who independently screened titles and abstracts against the inclusion/exclusion criteria and identified relevant papers. Then, the same two authors independently reviewed the full text studies unable to be excluded by title and abstract alone. Comparison of papers was completed between the two authors with no disagreements regarding inclusion.
Data extraction
The data extraction from final two articles was done using a data extraction form. It included the first author name, year of publication of the article, title, aim, study design, study population, data collection method, type of analyses, and results [Table 1].
| Author and Year | Title | Country, Journal, Publication | Aim | Study design and subjects, sampling method | Inclusion, Exclusion | Data collection method | Type of analyses | Result |
|---|---|---|---|---|---|---|---|---|
| Chhavi, 2011 | The prevalence of developmental defects of enamel in a group of 8–15 years old Indian children with developmental disturbances | Haryana, India, Journal of clinical and diagnostic research | Find out the prevalence of the DDE in disabled children | Cross sectional study, 118 subjects | Age 8–15 years. Disabled children included those students with special needs | Modified DDE index | Pearson’s Chi-square test | Prevalence of DDE among study group was 37.6% |
| Vesna Erika Modric, 2016 | Developmental defects of enamel in children with intellectual disability | Zagreb, Acta stomatol croat | Determine the frequency and distribution of DDE in children with intellectual disability | Cross sectional study, boys-84; girls-60 | Total of 72 children aged 5–18 years. Children whose molars have not erupted or were extracted were excluded from the study, as well as non-cooperative children and children who were not willing to participate in the study. | Modified DDE index | Chi-square or fisher extract | Study group was 27.78% |
Quality assessment
Articles included in data extraction were further assessed for quality using the Modified Newcastle-Ottawa scale.
In the modified Newcastle-Ottawa Quality Assessment Scale for cross-sectional studies, (1) group selection had 0–4 items, (2) comparability had 0–2 items, and finally, and (3) exposure had 0–3 items. Each study receives 1 point/each item. For part 1, the items include representativeness of the sample, sample size, non-respondents, and ascertainment of the exposure (risk factor). For part 2, the items nclude comparability for study control core factors and for additional factors, and for part 3, the items include assessment of outcome and statistical test. A maximum score of 5 points for group selection and exposure, 2 points for comparison group, and maximum of 3 points for outcome represents the highest methodological quality. The higher the score, better the quality of study [Table 2].
| Study | Chhavi Jindal et al., 2011 | Vesna Erica Modric et al., 2016 | |
|---|---|---|---|
| Selection and exposure | Sample representation | 1 | 1 |
| Sample size | 0 | 0 | |
| Non-respondents | 1 | 1 | |
| Ascertainment of exposure | 0 | 0 | |
| Outcome | Assessment of outcome | 0 | 2 |
| Statistical test | 1 | 1 |
RESULTS
Search results
The search generated a total of 56 articles from three different electronic bases: PUBMED, COCHRANE, and GOOGLE SCHOLAR. PUBMED produced 18 articles, COCHRANE produced nine articles and Google Scholar produced 29 articles.
The full texts of nine articles were obtained for further review. On basis of inclusion and exclusion criteria two articles were included in this systematic review. Full text of one article was not available on PubMed search. Author and year, study population, study design, objectives, inclusion and exclusion criteria, assessment tool, results, and summary of these included studies are tabulated in [Figure 1].
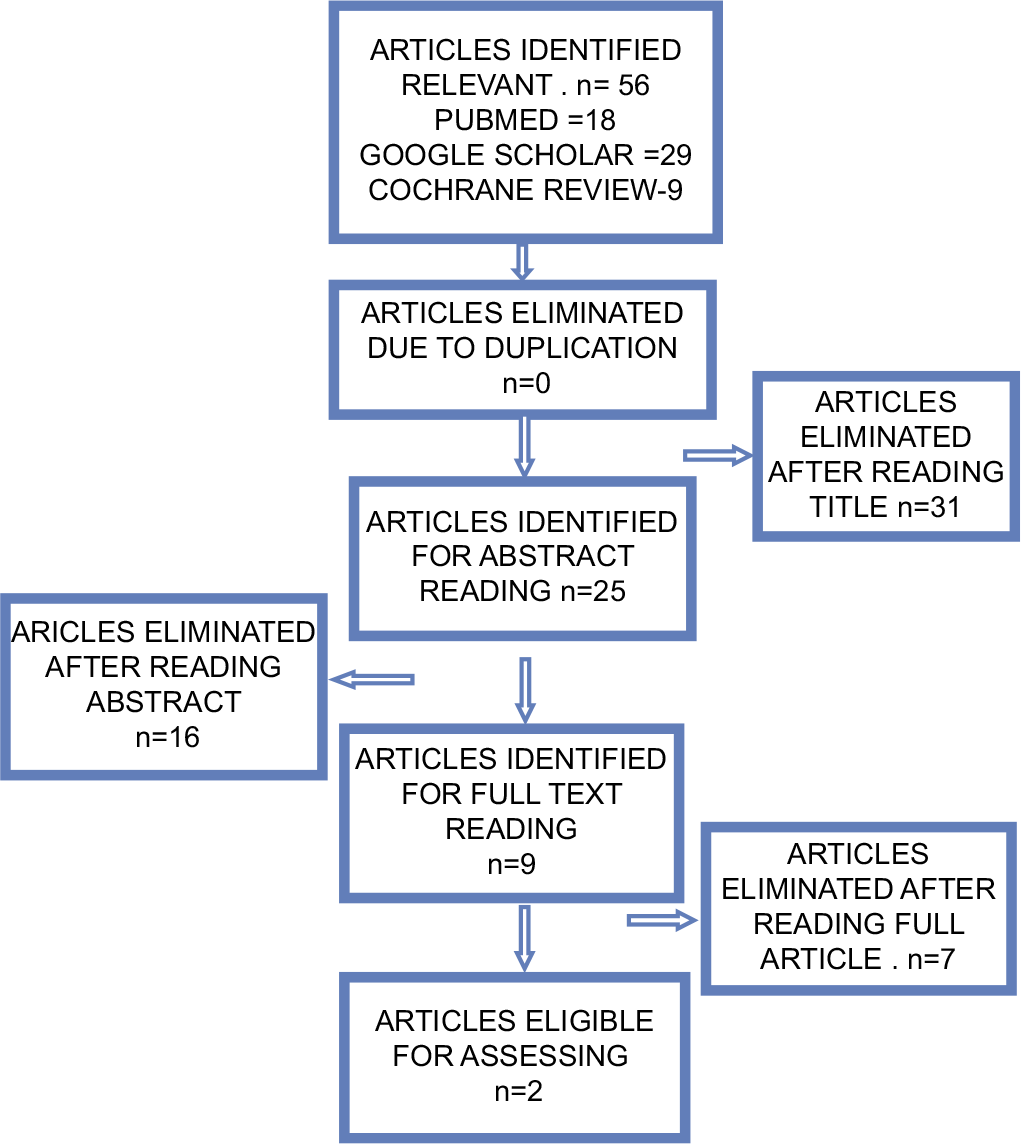
- Search procedure and exclusion criteria for the present review.
MAIN FINDINGS
Two included studies reported that the Developmental Defects of Enamel among ID children.
ASSESSMENT TOOL (OUTCOME)
Two studies utilized (MDDE) index to assess Developmental Defects of Enamel which was introduced by Clarkson and Mullane 1989. MDDE is a reliable tool consisting of six categories which includes normal, (1) demarcated opacities (2), diffuse opacities (3), hypoplasia (4), extent of defect (5), and combinations (6).
DISCUSSION
The main objective of this systematic review was to examine the prevalence of Developmental Defects of Enamel among ID.
Jindal et al. states that in general, a higher prevalence of enamel hypoplasia has been reported among malnourished children, very low birth weight children and in patients with sensort-neurological defects. The percent prevalence of the dental developmental defects of enamel among the intellectually disabled children was 37.6%.[7] Martinez et al., where 37.0% of the children with neurological disorders and mental retardation had the developmental defects of enamel. This could be attributed to the fact that several systemic disturbances which affect the neurological development also alter the development of the tooth germ. Because enamel cannot be recovered once it is damaged, it provides information on the timing and the nature of the insults which potentially affect other ectodermally derived structures like the brain. This study demonstrated (9.5%) of demarcated opacities in mentally retarded children and high prevalence (14.7%) of diffuse opacities.[8]
In the current study, among the disabled group, the developmental defects in the enamel were found to be highest in the maxillary incisors, followed by the mandibular incisors, the mandibular molars, the maxillary molars, the mandibular canines, the maxillary, and the mandibular premolars. The least affected was the maxillary canines. Suga et al. speculated that the ameloblasts which are responsible for the thick enamel were more susceptible to the systemic disorders than the ameloblasts which were associated with the thin enamel. The diffusion of calcium ions from the ameloblasts into the matrix and the removal of organic substances from the matrix are slower in the thick enamel than in the thin enamel. Hence, with thicker enamel, the teeth are exposed to the systemic injuries for a longer period of time.[9]
Erika et al. states that the prevalence of developmental defects of enamel in the permanent dentition was reported to be in the range of 2–63%. This review found that 27.78% of children with intellectual disabilities and 11.11% of healthy children had some type of DDE. On the other hand, the isolated opacities were found to be the most frequent type of enamel defect in our review on intellectual disabled children. Enamel hypoplasia was the most frequent type of enamel defect found. Most enamel defects were located on the anterior teeth and on the first permanent molars. Most enamel defects were distributed symmetrically. In this study, asymmetrically distributed defects were found in 60% of children with intellectual disabilities.[10] Trauma and infection of deciduous incisors can also cause opacities in the permanent incisors.[11,12]
Enamel defects are not only a cosmetic issue, but it could also be a retentive area which favors bacterial plaque accumulation and results in increased caries susceptibility. DDE may cause increased wear and tooth sensitivity which lead to pain and discomfort for the intellectual disabled child.[13] Enamel hypoplasia in deciduous teeth may also be predictive of similar disturbances in the permanent dentition. Yellow-brown defects have lower Knoop hardness values and greater porosity than the white defects and normal enamel. Even intact enamel of hypo mineralized molars may be very sensitive to air, cold, or warmth and children often avoid brushing the sensitive molars.[14-16] It is difficult for the children with intellectual disabilities to maintain good oral hygiene by themselves. They have impaired tooth-brushing ability and less patience due to their motor, sensor, and learning disabilities.
CONCLUSION
The results of this study showed that Developmental Defects of enamel was more common in ID children than normal children. Children with DDE should be identified because tissue loss and dental hypersensitivity increases caries risk, while reduced mechanical properties of hypo mineralized enamel often result in restoration failures. Hence, oral health promotion programs should be aimed at centers and schools for children with intellectual disabilities and should include the regular use of oral health services, oral hygiene education, and dietary counseling.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Intellectual developmental disorders: Towards a new name, definition and framework for “mental retardation/intellectual disability” in ICD-11. World Psychiatry. 2011;10:175-80.
- [CrossRef] [PubMed] [Google Scholar]
- An estimation of the prevalence of intellectual disabilities and its association with age in rural and urban populations in India. J Neurosci Rural Pract. 2015;6:523-8.
- [CrossRef] [PubMed] [Google Scholar]
- Prenatal, perinatal and neonatal risk factors for intellectual disability: A systemic review and meta-analysis. PLoS One. 2016;11:e0153655.
- [CrossRef] [PubMed] [Google Scholar]
- Developmental enamel defects in children born preterm: A systematic review. Eur J Oral Sci. 2014;122:7-14.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and distribution of developmental enamel defects in children with cerebral palsy in Beijing, China. Int J Paediatr Dent. 2011;21:23-8.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence of the developmental defects of enamel in a group of 8-15 years old Indian children with developmental disturbances. J Clin Diagn Res. 2011;5:669-74.
- [Google Scholar]
- Prevalence of developmental enamel defects in mentally retarded children. ASDC J Dent Child. 2002;69:151-5, 124
- [Google Scholar]
- Workshop on “Factors that influence the form and distribution of defects”. Adv Dent Res. 1989;3:99-100.
- [CrossRef] [Google Scholar]
- Developmental defects of enamel in children with intellectual disability. Acta Stomatol Croat. 2016;50:65-71.
- [CrossRef] [PubMed] [Google Scholar]
- Developmental enamel defects in the primary dentition: Aetiology and clinical management. Aust Dent J. 2013;58:133-40.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and association of developmental defects of enamel with, dental-caries and nutritional status in pre-school children, Lucknow. J Clin Diagn Res. 2015;9:ZC71-4.
- [CrossRef] [PubMed] [Google Scholar]
- Dental treatment, dental fear and behaviour management problems in children with severe enamel hypomineralization of their permanent first molars. Int J Paediatr Dent. 2002;12:24-32.
- [CrossRef] [PubMed] [Google Scholar]
- Molar-incisor hypomineralization and oral hygiene in 10-to-12-yr-old Swedish children born preterm. Eur J Oral Sci. 2011;119:33-9.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence of molar incisor hypomineralisation (MIH) in a group of Italian school children. Eur J Paediatr Dent. 2005;6:79-83.
- [Google Scholar]






