Tobacco cessation in India: Current trends, challenges, successes – A narrative review

*Corresponding author: Pramod Kumar Yadav, Department of Periodontia and Community Dentistry, Dr. Ziauddin Ahmad Dental College and Hospital, Aligarh Muslim University, Aligarh, Uttar Pradesh, India. pramod468@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Singh R, Nahid S, Mishra R, Ali A, Yadav PK. Tobacco cessation in India: Current trends, challenges, successes – A narrative review. J Global Oral Health. doi: 10.25259/JGOH_29_2024
Abstract
Tobacco use remains a significant public health challenge in India, despite various efforts aimed at cessation. This article synthesizes current trends, challenges, and successes in tobacco cessation based on the Global Youth Tobacco Survey (GYTS) 4, Global Adult tobacco Survey (GATS) 2, etc. The GYTS data highlights persistent high rates of tobacco use, that is, 8.5% of school going youth tobacco consumption, with the highest usage in Arunachal Pradesh and Mizoram (58% each), indicating a critical need for targeted interventions. Successes include the implementation of policies like Cigarette and Other Tobacco Product Act (COTPA), National Tobacco Control Program (NTCP), etc., which have shown initial positive impacts. About 21% of current smokers want to quit smoking now. However, challenges such as the cultural acceptance of tobacco use, socioeconomic disparities, and limited healthcare infrastructure pose significant barriers to effective cessation efforts. About 69% of current cigarette smokers bought cigarettes from a store, and 45% were not refused because of their age. The epidemiological perspective underscores the complex interplay of behavioral, social, and economic factors contributing to tobacco use, necessitating multifaceted approaches for cessation. Addressing these barriers requires comprehensive strategies that integrate community engagement, policy enforcement, and accessible healthcare services. Despite progress, sustained efforts are crucial to achieve substantial reductions in tobacco use prevalence and improve public health outcomes in India.
Keywords
Tobacco cessation
India
Global Youth Tobacco Survey
Global Adult Tobacco Survey
Public health
INTRODUCTION
Tobacco use is the leading single preventable cause of death globally, responsible for an estimated seven million deaths each year. On average, tobacco users lose 15 years of life, with up to half of all tobacco users dying prematurely due to tobacco-related causes. The majority of these deaths occur in middle and low-income nations, accounting for nearly 80% of all tobacco-related deaths. Despite its devastating impact, tobacco remains the most widely available and legally purchasable addictive substance. The Framework Convention on Tobacco Control (FCTC) is the most important global initiative for tobacco control, spearheaded by the World Health Organization (WHO). A key strategy to implement the FCTC is the MPOWER package, which consists of six evidence-based tobacco demand reduction measures. These include monitoring tobacco use and prevention policies, protecting people from tobacco smoke, offering help to quit tobacco use, warning about the dangers of tobacco, enforcing bans on tobacco advertising, promotion, and sponsorship, and raising taxes on tobacco.[1] Since the introduction of MPOWER and the start of its progress monitoring, there have been substantial advances in the adoption of robust tobacco control policies in all regions of the world and among countries of all income levels.
India is the third-largest tobacco-producing nation and the second-largest consumer of tobacco worldwide. Mortality due to tobacco in India is estimated to exceed 1.3 million annually, with one million deaths attributed to smoking and the rest to smokeless tobacco (SLT) use. A notable feature of tobacco-related mortality in India is the high incidence of oral cancer, surpassing even lung cancer and accounting for almost half of all oral cancers globally. India has the highest burden of both tuberculosis (TB) and multidrug-resistant TB, with smoking increasing the risk of TB by more than 2½ times. Smoking also contributes significantly to India’s rising burden of non-communicable diseases.
Recognizing the severe impact of tobacco use, the Indian government has initiated several measures to combat the tobacco epidemic. The regulatory action began in 2003 with the enactment of the Cigarettes and Other Tobacco Products Act (COTPA), which prohibits the advertisement and regulates the trade, commerce, production, supply, and distribution of tobacco products. India was one of the earliest nations to ratify the WHO FCTC in 2004 and launched its National Tobacco Control Program (NTCP) in 2007–2008. Smoking is now completely banned in most public places and workplaces, and all forms of tobacco advertising, promotion, and sponsorship are prohibited. It is also mandatory to have pictorial and text health warning labels on tobacco product packages. In 2014, the government mandated new larger warnings, increasing the warning size from 40% of one side of the packaging to 85% of both front and back panels. To ensure high-quality information on tobacco use to guide its control policies and programs, the Indian government has actively participated in global tobacco surveys, which are part of the Global Tobacco Surveillance System (GTSS). The major instrument for monitoring adult tobacco use and tracking key tobacco control indicators is the Global Adult Tobacco Survey (GATS).[2]
MATERIALS AND METHODS
The electronic search was conducted using publications from peer-reviewed journals and databases such as MEDLINE, ScienceDirect (Elsevier), PubMed, and others. The included articles’ reference list was then manually searched. Using different keywords and their permutations, such as tobacco cessation, India, GYTS, GATS, public health, and hurdles, web-based search engines such as Google Scholar were also utilized to extract pertinent papers. A total of 58 publications were located following an initial search that considered studies published in the recent several decades. Nevertheless, after a careful examination of each article, only 25 pertinent papers made it into the final analysis and abstracts.
Inhaling cigarette smoke exposes the cigarette smoker to over 7000 chemicals, which include the various tobacco constituents and the products of pyrolysis.[3] In India, it is one of the main causes of both sickness and mortality.[4] Although the link between smoking cigarettes and colorectal cancer is well established, the evidence supporting a direct relationship is weak.[5] For men, smoking is the primary cause of lung cancer fatalities at 90%, while for women, it is at 80%.[6] Active smoking has been shown to have a direct causal relationship with poor reproductive outcomes, cardiovascular illness, and chronic obstructive pulmonary disease.[5] Research conducted in India on bidi smoking, the most popular kind of tobacco use, points to the substance’s potential for cancer. Research on case-control populations shows a robust correlation between bidi smoking and malignancies of the mouth (including its subsites), throat, larynx, esophagus, lung, heart, and stomach. Regarding the length of time and quantity of bidis smoked, nearly all investigations exhibit noteworthy patterns.
Tobacco use damages the environment by causing the destruction of forests for agriculture, the removal of fuel wood for curing, and the extraction of natural resources for packing. Fast depletion of soil nutrients and displacement of native flora and animals by tobacco lead to pests that affect other crops.[7] Cigarette trash and e-cigarettes have the potential to enter the environment and contaminate water, air, and land with heavy metals, hazardous compounds, and leftover nicotine. A quarter of the carbon dioxide produced by commercial aircraft comes from the tobacco business, which emits 84 megatons of carbon dioxide annually.[8]
A 91% of the total economic burden was carried by men, with the remaining going to women. A 66% of the direct medical expenditures incurred by females are attributable to SLT. India is home to almost one-fifth of the world’s total production and cultivation of SLT, a growth pace that is concerning.[9] The primary addictive substance in tobacco that makes quitting difficult is nicotine. Nicotine gradually alters brain chemistry, giving the impression that a person needs nicotine to feel normal. Upon quitting smoking, your brain becomes agitated. You may find it difficult to focus or sleep, experience intense cravings for smoke, or simply feel uneasy all around. These are known as emotional withdrawal.[10] There is a link between smoking and some psychological issues.[11] There is minimal evidence about the significance of sociodemographic variables in relation to motives and barriers to stop smoking, despite some noteworthy findings. This is in contrast to the overall population.[12]
Behavioral therapies reorganize and transform mental processes in conjunction with tobacco users’ newfound learning habits and reliance to stop smoking and avoid relapsing. It also comprises embracing the cognitive therapy behavior principles involving yoga.[11] The effectiveness of therapy for tobacco dependency depends on counseling.
Individual and group counseling are useful tools for helping people with behavioral health disorders quit.[13] It is frequently required to undergo intensive behavioral therapy with longer and more frequent sessions. Using motivational interviewing and the five R’s system can also be effective.[14] Individuals who are trying to give up smoking should be urged to utilize the right medicine, either by itself or in certain combinations, unless there is an indication against it or if the patient belongs to a demographic for whom there is inadequate data supporting its efficacy.[14] The U.S. Food and Drug Administration has authorized seven first-line drugs, five of which are nicotine and two of which are non-nicotine. These treatments consistently raise the rates of long-term smoking cessation. Among them are bupropion SR, gum with nicotine, an inhaler for nicotine, a lozenge of nicotine, a nasal spray containing nicotine, and a varenicline-based nicotine patch.[14]
Replacing the substance with a safer and more therapeutically controllable form that directly relieves withdrawal symptoms and cravings is the general idea behind replacement therapy. nicotine replacement therapy (NRT) is based on protocols that were first created to treat opiate and heroin addiction. Numerous distribution methods that are not based on tobacco offer potentially efficient ways to replace nicotine.[15] Nicotine is incorporated into an ion exchange resin base in the “nicotine resin complex,” also referred to as nicotine gum. This allows nicotine to be released when the right amount of physical pressure chewing is applied in the right environment, which is saliva in the mouth. Ninety percent of the nicotine is released after 20–30 min of adequate chewing, while the exact amount of nicotine absorbed depends on a number of factors. A 10–15-min chewing period releases between 50% and 60% of the nicotine in a piece of gum.[16] Studies suggest that when compared to placebo controls, nicotine polacrilex gum lessens withdrawal symptoms.[17] The amount of nicotine that is truly gotten when using polacrilex gum is closely correlated with the level of alleviation.[18] Replacement of nicotine does not consistently lessen the craving or need to smoke.[19]
RESULTS
According to GATS 2, 266.8 million adults in India who are 15 years of age and older – 28.6% – currently use tobacco in some form. Adult tobacco users comprise 24.9% (232.4 million) daily users and 3.7% (34.4 million) infrequent users. The percentage of people who smoke varies by state and union territory (64.5% in Tripura and 9.7% in Goa). As per GATS 2, the most popular tobacco product in India is khaini, a tobacco and lime blend that is used by each adult every eighth (11.2%). Bidi is the second most popular tobacco product, smoked by 7.7% of adult Indians. In terms of usage, betel quid with tobacco ranks fourth (5.8%), whereas gutka – a mixture of tobacco, lime, and areca nuts – ranks third (6.8%), as given in Graph 1.[20]
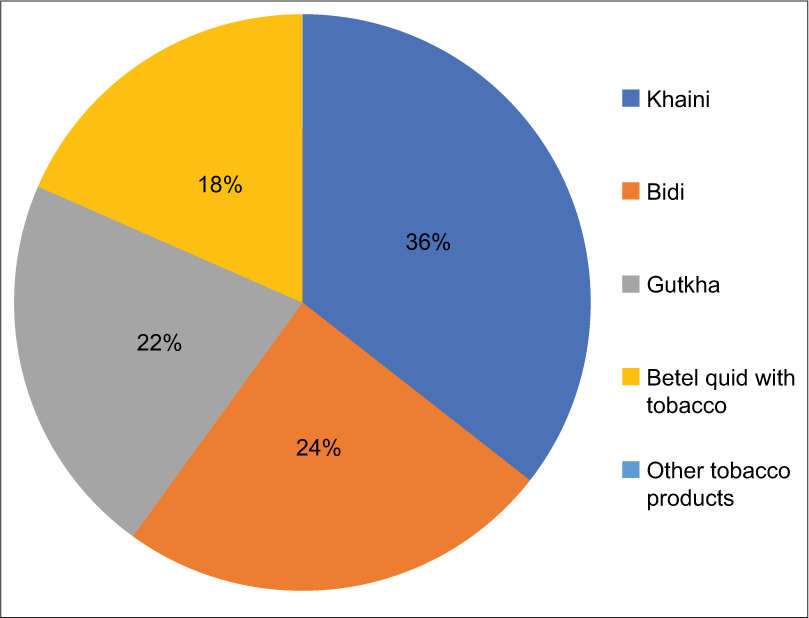
- Usage percentage of types of tobacco products in 15 years and above in Indians.
DISCUSSION
Significant drop in the usage of smokeless and smoked tobacco in all age groups, urban/rural areas, and genders. Second-hand smoke decreased exposure at home and public places but stagnation at workplaces. Anti-tobacco messaging increased the visibility of anti-tobacco messages on packs, encouraging more users to consider quitting. Some State variations show significant progress, while others need more efforts for effective tobacco control.
CONCLUSION
India has made positive strides in tobacco cessation, but obstacles still exist. With programs like the National Tobacco Control Programme (NTCP) and the implementation of tobacco product warnings helping to lower smoking rates, current trends show an increasing government commitment to tobacco control and awareness of the issue. Furthermore, community-based programs, helplines, and cessation clinics have effectively reached a wide range of people, demonstrating noteworthy achievements in providing support and increasing awareness. In order to increase access to cessation programs, enforce more stringent laws, and inform the public about the dangers of tobacco use, future success will require an integrated strategy involving the government, healthcare providers, non-governmental organizations, and community groups. While persistent governmental commitment and public awareness efforts are crucial for promoting a tobacco-free generation, innovations like digital health tools and mobile cessation support could bridge access gaps.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- 2018. Available from: https://www.mohfw.gov.in [Last accessed on 2024 Aug 17]
- Committee on the Public Health Implications of Raising the Minimum Age for Purchasing Tobacco Products, Board on Population Health and Public Health Practice, Institute of Medicine In: Bonnie RJ, Stratton K, Kwan LY, eds. Public Health implications of raising the minimum age of legal access to tobacco products. Washington, DC: National Academies Press (US); 2015. Ch. 4 Available from: https://www.ncbi.nlm.nih.gov/books/NBK310413 [Last accessed on 2024 Aug 17]
- [Google Scholar]
- Tobacco. Available from: https://www.who.int/india/health-topics/tobacco [Last accessed on 2024 Aug 17]
- [Google Scholar]
- Tobacco smoke and involuntary smoking In: IARC monographs on the evaluation of carcinogenic risks to humans. Lyon, FR: IARC; 2002. p. :83.
- [Google Scholar]
- A global epidemic of addiction and disease. Tobacco: deadly in any form or disguise, World Health Organization. WHO Tobacco Free Initiative In: World No Tobacco Day. 2006. Available from: https://www.who.int/tobacco/communications/events/wntd/2006/report_v8_4may06.pdf [Last accessed on 2011 Jun 17]
- [Google Scholar]
- Report on tobacco control in India (New Delhi, India) New Delhi, India: Ministry of Health and Family Welfare; 2004.
- [Google Scholar]
- Available from: https://ash.orguk/resources/view/tobacco-and-the-environment [Last accessed on 2024 Aug 17]
- Press release on tobacco 2014. Available from: https://www.searo.who.int/mediacentre/features/2014/taxing-tobaccoto-protect-the-health-poor/en/ [Last accessed on 2017 Oct 28]
- [Google Scholar]
- Tips from former smokers. Available from: https://www.cdc.gov/tobacco/campaign/tips/quit-smoking/quit-smoking-medications/why-quitting-smoking-is-hard/index.html#:~:text=you%20might%20have%20a%20hard,quit%2dsmoking%20medicines%20contain%20nicotine [Last accessed on 2024 Aug 17]
- [Google Scholar]
- Cognitive behavioral therapy for challenges to quitting tobacco smoking among social science and religion students. Medicine (Baltimore). 2022;101:e31913.
- [CrossRef] [PubMed] [Google Scholar]
- Motivations to quit smoking and challenges faced during cessation among individuals with first episode psychosis in Singapore. Early Interv Psychiatry. 2019;13:1488-94.
- [CrossRef] [PubMed] [Google Scholar]
- Yoga-enhanced cognitive behavioural therapy (Y-CBT) for anxiety management: A pilot study. Clin Psychol Psychother. 2015;22:364-71.
- [CrossRef] [PubMed] [Google Scholar]
- Available from: https://www.ncbi.nlm.nih.gov/books/NBK63952/ [Last accessed on 2024 Aug 17]
- Pharmacological basis for nicotine replacement In: Pomerleau OF, Pomerleau CS, Fagerstrom KO, Henningfield JE, Hughjes JR, eds. Nicotine replacement: A critical evaluation. New York: Alan R Liss; 1988.
- [Google Scholar]
- Pharmacotherapy of smoking cessation. Indian J Psychiatry. 2014;56:87-95.
- [CrossRef] [PubMed] [Google Scholar]
- Signs and symptoms of tobacco withdrawal. Arch Gen Psychiatry. 1986;43:289-94.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of nicotine replacement in tobacco withdrawal Washington DC: American Psychological Convention; 1986.
- [Google Scholar]
- Global adult tobacco survey GATS 2 India 2016-17. Available from: https://www.tiss.edu/view/11/research-projects/global-adult-tobacco-survey-round-2-for-india-2016 [Last accessed on 2024 Aug 17]
- [Google Scholar]






