Unraveling the association between oral impacts on daily performances and dental caries among adults in a South Indian Metropolis

*Corresponding author: Priya Babu, Department of Public Health Dentistry, Indira Gandhi Institute of Dental Sciences, Ernakulam, Kerala, India. priyaakhilesh0305@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Babu P, Amritha N, Ingale PC. Unraveling the association between oral impacts on daily performances and dental caries among adults in a South Indian Metropolis. J Global Oral Health. 2024;7:2-7. doi: 10.25259/JGOH_45_2023
Abstract
Objectives:
Conventionally, oral health outcomes have been assessed using clinical criteria and the subjective opinions of clinicians. However, these methods have failed to capture the true impact of oral diseases on an individual’s overall quality of life (QoL). Specifically, dental caries and tooth loss have been identified as factors that can significantly affect an individual’s oral health-related QoL (OHRQoL). Taking this into consideration, a recent study was conducted to investigate the association between oral impacts on daily performance (OIDP) scores and the oral health status of adults aged 25 years and older residing in Bengaluru South.
Materials and Methods:
A cross-sectional study was conducted among 800 adults aged 25 years and older in Bengaluru, South city. Clinical examination was performed using the decayed, missing-filled teeth (DMFT) index. OHRQoL was assessed using the OIDP questionnaire. For statistical analysis, the Chi-square test, Mann– Whitney U-test, Kruskal–Wallis test, and Spearman’s correlation were applied.
Results:
70.4% of the study participants had at least one oral impact affecting their daily performances. Out of eight daily performances, the most affected performance was eating, followed by emotional stability and carrying out major work. DMFT was significantly associated with OIDP.
Conclusion:
The prevalence of OIDPs in this population is high. Oral impacts had affected their QoL primarily through difficulties in eating. Appropriate program implementation is required for the upliftment of such deprived populations.
Keywords
Oral health-related quality of life
Dental caries
Oral impacts on daily performance (OIDP)
Decayed missing filled teeth (DMFT)
INTRODUCTION
Maintaining oral health is a fundamental aspect of overall health and well-being. It is an important factor that influences an individual’s quality of life (QoL).[1] Over time, the understanding of oral health has shifted from a biological approach to encompass social and psychological perspectives, acknowledging the varied roles of the oral cavity. This broader perspective also recognizes its impact on facial esthetics, self-esteem, communication, and social interactions.[2]
Dental caries is recognized as one of the most prevalent non-communicable diseases globally, with a 35% prevalence across all age groups, contributing significantly to the global burden of diseases.[3] Dental caries in India is also a significant public health burden affecting 60–65% of the population.[4]
In the field of dentistry, it has been acknowledged that relying solely on objective measures of disease offers limited insights into the influence of oral disorders on daily life and overall QoL.[5] Untreated oral symptoms, if allowed to persist, can significantly contribute to a decline in QoL.[2]
Many instruments have been developed for measuring oral health-related QoL (OHRQoL) during the past decades.[2] Among all the scales, oral impacts on daily performances (OIDPs) have acceptable psychometric properties, as well as a sound theoretical basis.[6] The OIDP assesses the presence of an oral problem, gauges its severity, and measures the extent to which the issue has negatively impacted the patient’s life.[7] It measures the physical, psychological, and social aspects of performances. Physical performance on the OIDP scale comprises eating, cleaning teeth, speaking, and doing physical activities; psychological performance includes sleeping, smiling, and emotional stability; and social performance comprises major role activity and contact with people.[6] It is ideal for use in cross-sectional surveys to discriminate between groups, assessing the impacts on individuals’ ability to perform daily activities.[8]
The assessment of how oral health influences QoL in adults remains a relatively neglected area in dental research in India. Although studies on OHRQoL have primarily concentrated on children and the elderly, there is a noticeable lack of research directed toward the adult population. Prioritizing research on assessing the OHRQoL in adults is crucial, as it provides insights into their expectations and can assist in tailoring effective strategies to address their concerns. Due to the limited number of published studies in India examining the association between oral health status and OIDP among adults, many of these studies have depended on samples sourced from dental institutions. Against this backdrop, the present study was initiated to examine the association between OIDP and oral health status, specifically within the adult population aged 25 years and above in Bengaluru -South.
MATERIALS AND METHODS
The present study is a cross-sectional study conducted on a sample of 800 subjects aged 25 years and above in Bengaluru city (South), Karnataka, India. A protocol for the study was submitted to the Institutional Ethical Committee, and the ethical clearance was obtained. The procedures followed in this study conformed to the ethical principles outlined in the Declaration of Helsinki.
Before the commencement of the study, the research protocol and objectives were explained, and informed consent was obtained from the study participants.
OIDP was pilot-tested among 30 subjects. The sample size required for the study was calculated to be 400, based on the results of a pilot study. Due to the heterogenecity in the population characteristics, a design effect of 2 was considered, and the sample size was inflated to 800.
The Bruhat Bengaluru Mahanagara Palike (BBMP), Greater Bengaluru Municipal Corporation oversees the civic administration of the city. BBMP divides Bengaluru into eight municipal zones, namely, Bommanahalli, Mahadevapura, Dasarahalli, Byatrayanpura, Raja Rajeshwari Nagar Zone, South Zone, West Zone, and East Zone. There are a total of 198 wards in these eight zones. South Bengaluru, which has 51 wards and is the biggest residential locality in Bengaluru, was selected for the study.
In our study, we employed a stratified cluster random sampling technique. Out of the 51 wards of South Bengaluru, ten wards were selected randomly which were treated as clusters. The survey was carried out to obtain a sample of 80 subjects from each cluster. Once 80 subjects from a particular ward were interviewed and examined; the next ward was sought until the desired sample size was achieved.
Inclusion criteria
The following criteria were included in the study:
Individuals aged 25 years or older
Participants who provided informed consent for participation in the study.
Exclusion criteria
The following criteria were excluded from the study:
Individuals with systemic medical conditions, neurological diseases, and mental disabilities
Edentulous individuals
Individuals with malocclusion
Individuals with dental fluorosis and severe wasting diseases or trauma.
A specially designed pro-forma was structured to gather information which consisted of four sections, namely, informed consent, respondent’s demographics, OHRQoL, and clinical examination. The OIDP instrument measures how oral disorders can have an impact on functioning, well-being, and QoL. This instrument has been validated in India[9] and used in various other studies.[7,10] It considers the self-perception of oral health conditions and its interference in daily activities in the past 6 months, based on dimensions of pain and discomfort, functional limitations, and dissatisfaction with appearance. The questionnaire also assessed the participant’s estimate of the frequency and severity of their difficulties. Frequency of the performances was recorded in the range- 0 = “never affected,” 1 = “less than once a month,” 2 = “once or twice a month,” 3 = “once or twice a week,” 4 = “3–4 times a week,” and 5 = “every or nearly every day.” Severity stands for how much the difficulty affects the participants’ daily lives. The severity scores range from 0 to 5, where 0 is “no effect” and 5 is “very severe effect.”[8] Test-retest reliability and internal consistency were checked for the questionnaire (0.87 and 0.85, respectively), and its validity was ensured before the start of the study.
The OIDP index assesses the impact of the oral condition on eight daily performances, namely, eating, speaking, cleaning the mouth, relaxing/sleeping, smiling, emotional stability, carrying out major work or social roles, and social contact. If a participant experienced an oral impact on any daily performance in the past 6 months, then its frequency and the severity of its effect were scored using 5-point ordinal scales. When a participant encountered an oral impact affecting any daily activity in the preceding 6 months, we utilized 5-point ordinal scales to score both the frequency and severity of its impact. A zero score was assigned if the participant reported no impact. The product of the respective frequency and severity scores determined the performance scores. An individual OIDP score was provided by dividing the sum of the eight scores by the possible maximum performance scores (performances [8] × maximum frequency score [5] and maximum severity scores [5] = 200). To provide a percentage score, the sum was multiplied by 100.[6]
A trained and calibrated examiner performed the clinical examination assessing signs for dental caries as recommended by the World Health Organization guidelines. To avoid interviewers’ bias, clinical examination and data collection were performed by a single trained examiner. Intra-examiner reliability, assessed by kappa statistic, was in the range of 0.78–0.82 for the parameters examined, showing a high degree of conformity.
Data were entered into Microsoft Excel, and analysis was done using the Statistical Package for the Social Sciences (SPSS) version 20 (IBM SPSS Statistics for Windows, IBM Corp, Armonk, NY, USA). Descriptive analysis of all study parameters was done using mean and standard deviation for continuous data and frequency and percentage for categorical data. Spearman’s correlation test was used to assess the relationship between OIDP score with clinical variables. Binary logistic regression was applied to check the relationship between OIDP as the dependent variable and decayed teeth and missing teeth as an independent variable. P < 0.05 was considered as statistically significant.
RESULTS
The final sample included 800 participants aged 25 years and above, comprising 389 (48.6%) males and 411 (51.4%) females. Table 1 displays the distribution of study participants based on age. Most of the participants were in the 25–34 year age group.
About 225 (28.1%) participants did not exhibit any caries experience (decayed missing filled teeth [DMFT] score = 0), whereas 575 (71.9%) had a DMFT score above 1. Among the 800 participants, 509 (63.6%) had decayed teeth, 261 (32.6%) had missing teeth, and 90 (11.3%) had filled teeth. The mean DMFT was obtained to be 3.15 ± 3.38. The mean DMFT score was higher in the age group equal to or greater than 55 years (5.92 ± 5.64), followed by 45–54 years (3.53 ± 3.43) and least in 35–44 years (2.61 ± 2.68), and the results were found to be statistically significant (P < 0.001).
| Age groups | Males | Females | Total |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| 25–34 years | 164 (42.1) | 150 (36.5) | 314 (39.2) |
| 35–44 years | 92 (23.7) | 155 (37.7) | 247 (30.9) |
| 45–54 years | 93 (23.9) | 68 (16.5) | 161 (20.1) |
| ≥55 years | 40 (10.3) | 38 (9.3) | 78 (9.8) |
| Total | 389 (100) | 411 (100) | 800 (100) |
Assessment of the prevalence of OIDP showed that 70.4% of study participants experienced one or more oral impacts on their daily performances in the past 6 months. [Figure 1] shows the prevalence of the eight oral impacts on the daily performance of the sample.
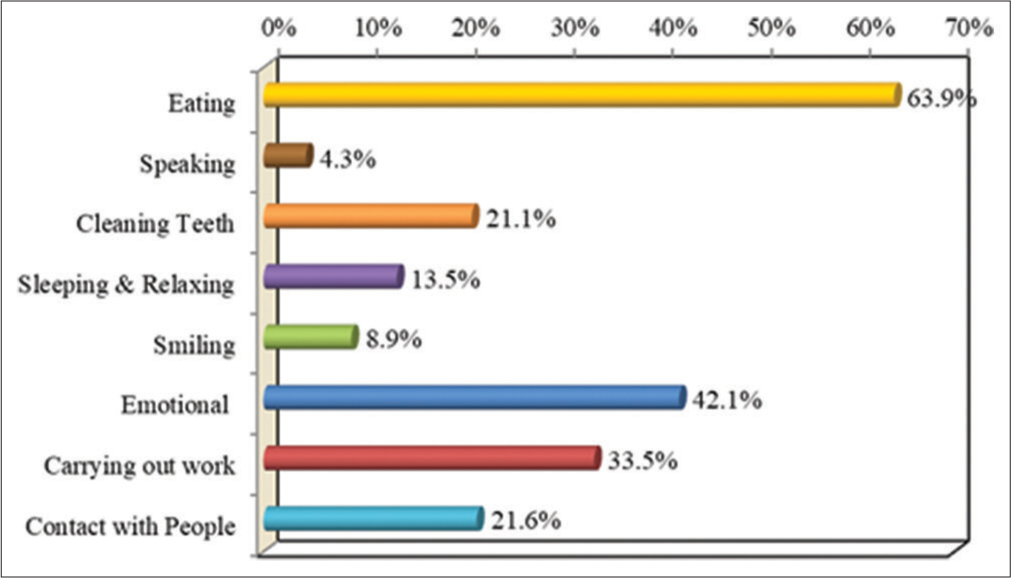
- Prevalence of oral impact on daily performances.
Table 2 shows the association of OIDP items based on DMFT among study participants. Study participants with DMFT score ≥1 are 2.4 times more affected in eating, 1.38 times more affected in sleeping and relaxing, 1.15 times more affected in smiling, 1.54 times more affected in maintaining usual emotional state, 1.50 times more affected in carrying out major work, and 1.39 times more affected in social contact with people as compared to study participants with DMFT = 0. The results were statistically significant (P < 0.001).
There was a positive correlation between OIDP total score and decayed teeth (r = 0.55), missed teeth (r = 0.31), and DMFT scores (r = 0.54) [Table 3].
| OIDP items | Category | DMFT=0 | DMFT≥1 | OR | P-value | ||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Eating | Yes | 61 | 27.1 | 450 | 78.3 | 2.40 | <0.001* |
| No | 164 | 72.9 | 125 | 21.7 | |||
| Speaking | Yes | 1 | 0.4 | 33 | 5.7 | 1.37 | <0.001* |
| No | 224 | 99.6 | 542 | 94.3 | |||
| Cleaning Teeth | Yes | 41 | 18.2 | 128 | 22.3 | 1.07 | 0.25 |
| No | 184 | 81.8 | 447 | 77.7 | |||
| Sleeping and Relaxing | Yes | 6 | 2.7 | 102 | 17.7 | 1.38 | <0.001* |
| No | 219 | 97.3 | 473 | 82.3 | |||
| Smiling | Yes | 13 | 5.8 | 58 | 10.1 | 1.15 | <0.001* |
| No | 212 | 94.2 | 517 | 89.9 | |||
| Emotional | Yes | 33 | 14.7 | 304 | 52.9 | 1.54 | <0.001* |
| No | 192 | 85.3 | 271 | 47.1 | |||
| Carrying out work | Yes | 21 | 9.3 | 247 | 43.0 | 1.50 | <0.001* |
| No | 204 | 90.7 | 328 | 57.0 | |||
| Contact with people | Yes | 14 | 6.2 | 159 | 27.7 | 1.39 | <0.001* |
| No | 211 | 93.8 | 416 | 72.3 | |||
| Clinical variables | Overall OIDP scores | |
|---|---|---|
| Rho | P-value | |
| Decayed teeth | 0.55 | <0.001* |
| Missing teeth | 0.31 | <0.001* |
| Filled teeth | 0.02 | 0.52 |
| DMFT | 0.54 | <0.001* |
DISCUSSION
Oral diseases were generally not fatal, but they had the potential to influence the “ability to eat, speak, and socialize.” Certainly, oral disorders have the potential to impact interpersonal relationships and daily activities, consequently influencing the overall “goodness” or “quality of life.”[11] The impact of oral diseases on the QoL is obvious. Any illness that disrupts the routine activities of daily life may adversely affect one’s general QoL.[2] Conventional approaches to measuring oral health predominantly rely on clinical dental indices, concentrating on determining the presence or absence of oral diseases. However, these dental indices do not provide insights into individuals’ OHRQoL. The shortcomings associated with the normative approach in assessing oral health have prompted the development of measures related to OHRQoL.[12] It has garnered substantial attention from both academics and the public. In this study, the concepts of OHRQoL were examined through the lens of an individual’s perception of the impacts of oral diseases on their daily activities. This assessment was conducted using the OIDP instrument. The OIDP is one of the most widely used socio-dental indicators, which focuses on measuring serious oral impacts on a person’s ability to perform daily activities.[13] There is scarce literature related to OHRQoL among the general population of India. Indeed, many of the QoL indicators in dentistry have focused primarily on older age groups and children.
In the present study, a substantial occurrence of oral impacts was observed, with 70.4% of the participants experiencing at least one oral impact that influenced their daily life in the past 6 months. This prevalence in our study was slightly lower than that reported by Purohit et al., 72% who assessed the prevalence of oral impacts in adults who attended the dental outreach center in the Udupi district.[9] These differences can be explained by the fact that the present study was performed on the general population rather than the participants who visit a dental outreach center, which sees more dental problems compared to the general population. These findings are corroborated by a previously published study conducted by Montero et al.,[14] which revealed a higher prevalence of impacts in Spanish dental patients when compared to the general Spanish population. A study conducted by Moeintaghavi et al.,[8] reported a higher prevalence of oral impacts, that is, 84% among adults living in Mashhad, Iran, and Mohebbi et al.,[15] also reported a higher prevalence of 82.6%. The variations in the occurrence of oral impacts within the population may stem from socioeconomic and cultural differences or disparities in oral health status.
The present study revealed “eating” to be the most prevalent daily activity affected by oral problems, which is in line with the results of several studies in different populations such as Åstrøm et al.,[16] Purohit et al.,[9] Chowdary et al.,[17] Peker and Alkurt,[18] Montero et al.,[14] and Dorri et al.,[10] where the researchers identified eating as the predominant activity impacted by negative oral conditions. This finding highlights the importance of the physical aspects of the teeth and mouth in participants’ lives.
Study participants with DMFT >0 showed a significant association with having one or more impacts on daily physical, psychological, and social performances in this population. This shows the severe impacts of oral health on QoL. A study conducted by Leão et al.,[19] also reported that participants having DMFT >0 had a major impact on social relationships. In the present study, the correlation between OIDP score and DMFT showed a significant positive relationship, which was in line with the studies conducted by Bakhtiar et al.,[20] and Simangwa et al.,[21] However, Chowdary et al.,[17] Purohit et al.,[9] and Sirohi et al.,[22] did not find a statistically significant relationship between DMFT and OIDP.
The present study found that participants with dental caries were more likely to report their oral conditions as having impacted their daily performances compared to those without dental caries. The pain that accompanies dental caries invariably draws the attention of the individual, leading to significant influences or impacts on their daily performances. These findings were similar to the studies done by Lawal et al.[23] and Andersson et al.[24] Correlation between decayed teeth and OIDP score had shown a significant positive interrelation. This finding is in agreement with the study conducted by Dhama et al.,[25] in which a statistically significant positive correlation was found between decayed teeth and OIDP score. Refuting findings were seen in a study conducted by Soe et al.,[26], where the number of decayed teeth was not correlated with the total OIDP score.
Contrary findings were noted in the study conducted by Andersson et al.,[24], where researchers did not observe a statistically significant relationship between missing teeth and OIDP scores. This discrepancy may be attributed to the low frequency of missing teeth among the participants in their study.
The clinical indicators available for our analyses are important markers for oral health and function of adults, and the study is stronger as more extensive clinical information is available, such as the presence of caries and missing teeth. From a public health point of view, our results highlight the importance of OHRQoL. The present findings can be generalized to populations with cultural and demographic characteristics like the population that lives in south Bengaluru.
There are certain limitations in our study. The cross-sectional design of the study poses a challenge in evaluating risk predictors of OHRQoL. The use of the OIDP inventory, with a recall period of 6 months and reliance on self-reports, introduces the possibility of recall bias. It’s important to note that longer recall periods, unlike shorter ones, may lead to underestimation of health consequences. However, it is also recognized that longer recalls could provide valid estimates for severe outcomes.
Future research should focus on determining how measures of OHRQoL can be integrated into treatment needs estimation systems, providing valuable insights for the planning and delivery of services. This could enhance the overall effectiveness and responsiveness of oral health-care programs. Intervention studies are needed to assess whether dental care reduces the impacts and affects the QoL.
CONCLUSION
The OIDPs were highly prevalent among our participants, indicating that oral problems had a significant impact on their daily activities. The presence of a strong and consistent association between OHRQoL and dental caries suggests a clear link between the impact of dental caries and individuals’ overall well-being. The provision of dental care to adults should address not just their clinical dental needs but also their perceptions in terms of the impact of oral conditions on their daily lives.
Ethical approval
The research/study approved by the Institutional Review Board at AECS Maaruti College of Dental Sciences and Research Centre, number 196/2016–17, dated November 23, 2016.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Oral health, general health, and quality of life. Bull World Health Organ. 2005;83:644.
- [Google Scholar]
- Oral health-related quality of life: A broader perspective. East Mediterr Health J. 2006;12:894-901.
- [Google Scholar]
- The global burden of oral diseases and risks to oral health. Bull World Health Organ. 2005;83:661-9.
- [Google Scholar]
- National oral health survey and fluoride mapping 2002-2003 India New Delhi: Dental Council of India; 2004. p. :100-6.
- [Google Scholar]
- Oral health-related quality of life in Swedish young adults. Int J Qual Stud Health Well-being. 2015;10:27125.
- [CrossRef] [PubMed] [Google Scholar]
- Measuring oral health and quality of life United States: Department of Dental Ecology, School of Dentistry, University of North Carolina; 1997.
- [Google Scholar]
- Development of a Japanese version of the Oral Impacts on Daily Performance (OIDP) scale: A pilot study. J Oral Sci. 2007;49:259-64.
- [CrossRef] [PubMed] [Google Scholar]
- Oral health-related quality of life: A cross-sectional survey among adult patients in Mashhad, Iran. J Dent Mater Tech. 2013;2:114-20.
- [Google Scholar]
- Assessment and validation of the oral impact on daily performance (OIDP) instrument among adults in Karnataka, South India. Community Dent Health. 2012;29:203-8.
- [Google Scholar]
- Validation of a Persian version of the OIDP index. BMC Oral Health. 2007;7:2.
- [CrossRef] [PubMed] [Google Scholar]
- Oral health related quality of life in adult population attending the outpatient department of a hospital in Chennai, India. J Int Oral Health. 2010;2:45-56.
- [Google Scholar]
- The prevalence and severity of oral impacts on daily performances in Thai primary school children. Health Qual Life Outcomes. 2004;2:57.
- [CrossRef] [PubMed] [Google Scholar]
- Oral health status and oral impact on daily performance in elderly in Northeastern region Thailand. Eur J Sustain Dev. 2017;6:240.
- [CrossRef] [Google Scholar]
- Oral health-related quality of life of a consecutive sample of Spanish dental patients. Med Oral Patol Oral Cir Bucal. 2011;16:e810-5.
- [CrossRef] [PubMed] [Google Scholar]
- Oral impacts on daily performance in 20-to 50-year-olds demanding dental care in Tehran, Iran: Association with clinical findings and self-reported health. Oral Health Prev Dent. 2014;12:29-36.
- [Google Scholar]
- Oral impacts on daily performance in Norwegian adults: The influence of age, number of missing teeth, and socio-demographic factors. Eur J Oral Sci. 2006;114:115-21.
- [CrossRef] [PubMed] [Google Scholar]
- Oral impacts on daily performances in white-collar port workers in Nellore, India-A cross-sectional study. Int Marit Health. 2016;67:205-13.
- [CrossRef] [PubMed] [Google Scholar]
- Oral impacts on daily performance in Turkish adults attending a dental school. J Contemp Dent Pract. 2014;15:92-8.
- [CrossRef] [PubMed] [Google Scholar]
- Oral health and quality of life: An epidemiological survey of adolescents from settlement in Pontal do Paranapanema/SP, Brazil. Cien Saude Colet. 2015;20:3365-74.
- [CrossRef] [PubMed] [Google Scholar]
- Association of oral health indicators with quality-of-life related to oral health among Iranian adolescent. J Int Oral Health. 2014;6:5.
- [Google Scholar]
- Oral impacts on daily performances and its socio-demographic and clinical distribution: A cross-sectional study of adolescents living in Maasai population areas, Tanzania. Health Qual Life Outcomes. 2020;18:181.
- [CrossRef] [PubMed] [Google Scholar]
- Oral health related quality of life in adult population attending outpatient Department of KD Dental College and Hospital, Mathura. J Oral Health Community Dent. 2015;9:30-4.
- [CrossRef] [Google Scholar]
- Impact of oral health on the quality of life of elementary school teachers. Ethiop J Health Sci. 2015;25:217-24.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of oral health on daily performances and its association with clinical variables in a population in Zambia. Int J Dent Hyg. 2017;15:128-34.
- [CrossRef] [PubMed] [Google Scholar]
- Magnifying the senescence: Impact of oral health on quality of life and daily performance in geriatrics: A cross-sectional study. J Int Soc Prev Community Dent. 2017;7(Suppl 2):S113.
- [CrossRef] [PubMed] [Google Scholar]
- Reliability and validity of two oral health related quality of life measures in Myanmar adolescents. Community Dent Health. 2004;21:306-11.
- [Google Scholar]






