Translate this page into:
Post-cheilorhinoplasty esthetic evaluation of unilateral cleft lip and palate infants treated with and without pre-surgical nasoalveolar molding

*Corresponding author: Navdeep Bhusri, Department of Craniofacial Orthodontics, New World Medical Center, Phnom Penh, Cambodia nav_bhusri@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Bhusri N, Lim DC, Pandan MM. Post-cheilorhinoplasty esthetic evaluation of unilateral cleft lip and palate infants treated with and without pre-surgical nasoalveolar molding. J Global Oral Health 2023;6:85-90.
Abstract
Objectives:
Unilateral cleft lip and palate sets many challenges both functional and esthetic. Cleft patients are at an elevated risk for developing psychosocial problems. The objective of this study was to assess any difference in esthetics post-cheilorhinoplasty in unilateral cleft lip and palate (UCLP) infants treated with and without nasoalveolar molding.
Materials and Methods:
Esthetic evaluation of nasolabial appearance and comparative analysis of photographic records collected post-cheilorhinoplasty for presurgical nasoalveolar molding (PNAM), lip-tape (LPTP), no pre-treatment (NoPreTx), and control (CTRL) groups were done using 5 point scale. There were six evaluators, two orthodontists, and one maxillofacial surgeon each from the two participating institutions. Paired “t”-test for nasolabial score comparison between groups, Cronbach’s alpha for reliability analysis, and Fleiss Kappa for interevaluator agreement were used for statistics. All statistical analysis was done at confidence level of 95% and 0.05 as level of significance.
Results:
Significant difference was found between nasolabial esthetic scores for PNAM group when compared to LPTP (P = 0.000) and NoPreTx (P = 0.001) groups. Infants who underwent PNAM had better nasolabial esthetic scores in all categories compared to infants who underwent LPTP or NoPreTx. The scale of measurement and the nasolabial esthetic evaluation scores were coherent and reliable as shown by Crohnbach’s alpha (<0.9) both for individual components and for overall score.
Conclusion:
UCLP infants who were brought by their parents to the craniofacial center early within 1 month of their birth and who underwent nasoalveolar molding therapy before cheilorhinoplasty had significantly better nasolabial esthetics post-surgery.
Keywords
Cleft lip/diagnostic imaging
Cleft lip/therapy
Orthodontics/corrective
Cleft lip/surgery
Reconstructive surgical procedures/esthetic
INTRODUCTION
The incidence of cleft lip and palate in the Philippines has been reported to be 1.94/1000 live births which is consistent with other, previously-reported rates for Asian populations and supports the observation of higher incidences of clefting in Asian populations when compared to Caucasian populations. The index of treatment need developed by Brook and Shaw places defects of cleft lip and palate and other craniofacial anomalies on a Grade 5 (extreme/need treatment).[1] Adolescents with cleft palate/lip are at an elevated risk for developing psychosocial problems especially those relating to self-concept, peer relationships, and appearance. “The term unilateral cleft lip is almost a misnomer because nearly always the nose is an integral part of the problem that must be addressed to obtain an improved result.”[2] “The wider, more extensive clefts are associated with more significant nasolabial deformity and most surgeons would agree that their chance of achieving a finer surgical scar, good nasal tip projection, and more symmetrical and precisely defined nasolabial complex would be better in an infant who presents with a minor cleft deformity.”[3] The cleft lip and palate deformities are complex with the involvement of not only the palate and lip but also the nose. The shape of the nose gets affected in all the three planes of space. The deformity appears as distortion, displacement, and tissue deficiency of nasal and maxillary structures.
As a result, the following features [Figures 1a and b] can be seen clinically in complete unilateral cleft lip and palate (CUCLP):
“Tilted tripod” nasal deformity
Premaxilla on the non-cleft side turned out
Lower lateral alar cartilages on the cleft side are abnormally stretched with inferior and medial rotation
Horizontal nostril aperture on the cleft side
Depressed cleft nasal dome
Distorted and short cleft columella
Septum deviated toward the non-cleft side
Orbicularis oris muscle in the lateral lip segments contracts into a bulge with some fibers running superiorly along the margin of cleft toward nasal tip.

- Features of unilateral cleft lip and palate infant, (a) frontal view showing the “Tilted tripod” nasal deformity, premaxilla on the non-cleft side turned out, and horizontal nostril aperture on the cleft side (b) basilar view showing the depressed cleft nasal dome, deviated, and short cleft columella.
The standard treatment protocol for the cleft lip and palate patients remains a subject of debate. There are two main school of thoughts, one involving surgical repair alone and the other involving pre-surgical molding of the cleft segments followed by surgical repair.[4] Pre-surgical infant orthopedics (PSIO) has been on the scene since 1950s as an adjunctive neonatal therapy for the correction of cleft lip and palate when McNeil first introduced the concept of modern pre-surgical orthopedics.[5] The presurgical nasoalveolar molding (PNAM) treatment is based on the study by Matsuo inferring that the nasal cartilage is developing, lacks elasticity, and is still tenable to molding within neonatal period (first 6 weeks), and applied this principle to mold nostrils of infants using silicon tubes.[6] PNAM was first described by Dr. Grayson from New York University.[7]
Biomechanics of PNAM involves repositioning the maxillary segments [Figures 2a-c] by bringing the lip segments into closer approximation to each other and also correcting the nasal deviation, thus making it easier for the surgeons enabling a more precise lip and nasal repair with less tension. However, no valid research exists to demonstrate that better esthetic results follow post-cheilorhinoplasty in infants treated with PNAM. The objective of this study was to assess if there were any significant differences in esthetics post-cheilorhinoplasty in unilateral cleft lip and palate (UCLP) infants treated with or without PNAM.

- Presurgical nasoalveolar molding (PNAM) therapy for unilateral cleft lip palate, (a) before PNAM therapy infant with wide lip/alveolar cleft and deviated columella; (b) PNAM biomechanics with acrylic bulb raising the nasal dome and centering the columella, lip tape providing the force for approximation of cleft lip and alveolar gaps; and (c) after PNAM therapy showing overcorrected nasal dome and minimal cleft lip/alveolus gap.
MATERIALS AND METHODS
This research study was prospective and exploratory in nature. The major part of this research, nasoalveolar molding, photographs, cheilorhinoplasty, and data collection, was conducted in a craniofacial center attached to a hospital. The descriptive data recorded for each subject included parameters of gender, side of the cleft, age (in weeks) of start of PNAM and lip-tape (LPTP), active period of NAM and LPTP, age (in weeks) at the time of cheilorhinoplasty for all groups, and of control (CTRL) group.
The sampling design was non-probability purposive sampling method wherein elements were chosen based on purpose of the study and were representative of only a subset of the whole population, which, in this particular study, were UCLP patients. This kind of sampling method is suitable for in-depth qualitative research in which the focus is often to understand complex phenomena.[8]
Applying formula for two sample computations of proportions, keeping confidence level (Za/2) at 95% (1.96); desired power (Zb) at 80% (0.84); size of difference of clinical importance of PNAM treatment (∩1-∩2), at 80%(∩1)-15%(∩2), that is, 0.65 (reducing cleft gap by at least 65% from 6 to 2 mm);
N = {(Za/2+Zb)2 × (∩1[1-∩1]+∩2[1-∩2])}/(∩1-∩2)2
We obtain sample size, n = 5.3349 (≈6) per group. In this study, the sample size of 26 (PNAM+LPTP+NoPreTx+CTRL) meets the minimum criterion of samples required as computed above. The duration/length of involvement of each subject/participant was at least 2 months adhering to given time points i1, i2, and i3 (each appointment took 30–45 min).
Four groups were studied, first being PNAM group with six infants who underwent PNAM therapy with cheilorhinoplasty, second was LPTP group with six infants who underwent LPTP therapy with cheilorhinoplasty, third group was NoPreTx with seven infants who underwent NoPreTx with cheilorhinoplasty only, and CTRL or CTRL group which included seven normal infants without any craniofacial and/or systemic condition.
The following criteria were included in the study:
Complete unilateral cleft lip, alveolus, and palate (PNAM, LPTP, and NoPreTx)
Maximum 6 weeks of age at start of PNAM
At least 3 months and 5 kg (PNAM, LPTP and NoPreTx) for cheilorhinoplasty.
The following criteria were excluded from the study:
Clefts patients with syndromes or other systemic disorders, etc.
Patients above 6 weeks at the start of PNAM
Patients above 6 months for NoPreTx
Non-compliant subjects for more than 1 appointment missed or PNAM not used.
Methodology
Nikon D3100 DSLR camera was used with AF-S NIKKOR 18–55 mm 1:3.5–5.6 G lens system for extraoral photographs of the infants. All the photographic records were taken from a distance of 1 foot [Figure 3].

- Photographic record taken at a distance of 1 foot using Nikon D3100 DSLR 18–55 system with through the lens macro flash.
The photographs for the area of the interest, upper lip and nose only, in both frontal and basilar views were taken at three time points:
i1 – Before cheilorhinoplasty
i2 – 1 week after cheilorhinoplasty on the day of suture removal
i3 – 1 month after cheilorhinoplasty when wound attains adequate strength.
All the photographic plates were made gray scale and other facial features of the infants such as eyes, ears, and chin not included in the photographs evaluated to prevent bias in the scoring of the evaluators toward a more beautiful full face [Figures 4a and b].

- Gray scale photographic records with only area of interest shown for evaluation, (a) frontal view of a patient at time point i3 and (b) basilar view of a patient at time point i3.
Esthetic evaluation of nasolabial appearance for groups PNAM, LPTP, NoPreTx, and the CTRL was done on postsurgical photographic records collected at time point “i3” using 5 point scale grading system.[9] Four esthetic components were studied namely nostril form (a), nasal deviation (b), nasal form (c), and vermillion area (d). The appearance was evaluated on a 5 point scale with scoring criteria as very good (1), good (2), regular (3), poor (4), and very poor (5). A Green Flag category (Very Good + Good scores) and a Red Flag category (Poor + Very Poor scores) were devised for this study for overall absolute demarcation of esthetic scores [Table 3].
Approval for use of the clinical records was obtained from the medical director of the craniofacial center and university ethical review committee clearance obtained vide study protocol approval code 0201/E/O/14/064. The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000.
The data underwent descriptive statistics for the patient sample involved. The individual and overall nasolabial esthetic evaluation scores underwent frequency distributions among groups PNAM, LPTP, NoPreTx, and CTRL. Differences in nasolabial esthetic scores among the four groups were computed using a two-tailed Paired “t”-test. Internal consistency estimate of reliability for the nasolabial esthetic evaluation scores or reliability of the scale of measurement was checked using Cronbach’s alpha. Interevaluator agreement of the nasolabial esthetic evaluation scores was checked using Fleiss Kappa. All statistical analysis was done with SPSS statistical software V17.0 (SPSS Inc., Chicago) at a confidence level of 95% and 0.05 level of significance.
RESULTS
The descriptive characteristics of research subjects and mean ages (weeks) for each group are tabulated in Tables 1 and 2, respectively. The mean age at start of PNAM therapy was 2.47 (1.77) weeks which was within 1st month of birth.
| n | Male | Female | Side of Cleft | ||
|---|---|---|---|---|---|
| Left | Right | ||||
| UCLP | 19 | 12 | 7 | 12 | 7 |
| CTRL | 7 | 4 | 3 | n/a | n/a |
UCLP: Unilateral cleft lip and palate (Cleft groups), CTRL: Control group, *n= No. of subjects in each category.
| Mean age (SD) | Start of presurgical therapy | Active PNAM period | Cheilorhinoplasty | Evaluation of CTRL group |
|---|---|---|---|---|
| PNAM | 2.47 (1.77) | 10 (1.41) | 13 (1.09) | n/a |
| LPTP | 8.5 (1.26) | 5.33 (1.21) | 14.16 (0.98) | n/a |
| NoPreTx | n/a | n/a | 17.85 (1.75) | n/a |
| CTRL | n/a | n/a | n/a | 12.64 (0.75) |
SD: Standard deviation, PNAM: Presurgical nasoalveolar molding, LPTP: Liptape, NoPreTx: No pre-treatment/only cheilorhinoplasty, CTRL: Control, n/a = not applicable
| PNAM (%) | LPTP (%) | NoPreTx (%) | CTRL (%) | |
|---|---|---|---|---|
| A (1+2) | 40.28 | 23.62 | 23.81 | 100 |
| A (4+5) | 27.78 | 52.77 | 42.86 | 0 |
| B (1+2) | 47.22 | 26.38 | 24.68 | 98.80 |
| B (4+5) | 23.61 | 33.34 | 29.62 | 0 |
| C (1+2) | 34.72 | 12.50 | 22.62 | 83.33 |
| C (4+5) | 30.56 | 40.28 | 40.47 | 0 |
| D (1+2) | 25 | 15.28 | 22.62 | 94.05 |
| D (4+5) | 33.34 | 41.66 | 41.67 | 0 |
A: Nostril form, B: Nasal deviation, C: Nasal form, D: Vermillion border; Green Flag category (1+2)=(Very Good + Good), Red Flag category (4+5)=(Poor + Very Poor). PNAM: Presurgical nasoalveolar molding, LPTP: Liptape, NoPreTx: No pre-treatment/only cheilorhinoplasty, CTRL: Control
Percentage frequency of nasolabial esthetic scores is presented in Figures 5a-d. For the nostril form (a), nasal deviation (b), and nasal form (c) components, PNAM group got the maximum scores in the very good (1) category. For the Vermillion Border (D) component, the evaluators gave Regular (3) scores most often for PNAM, LPTP, and NoPreTx groups. For cumulative percentages in Green Flag category, PNAM group got the highest percentage of good scores for all nasolabial esthetic components and in the Red Flag category, LPTP group got the worst scores for esthetic components A and B, whereas group NoPreTx had bad scores than LPTP for esthetic components C and D.
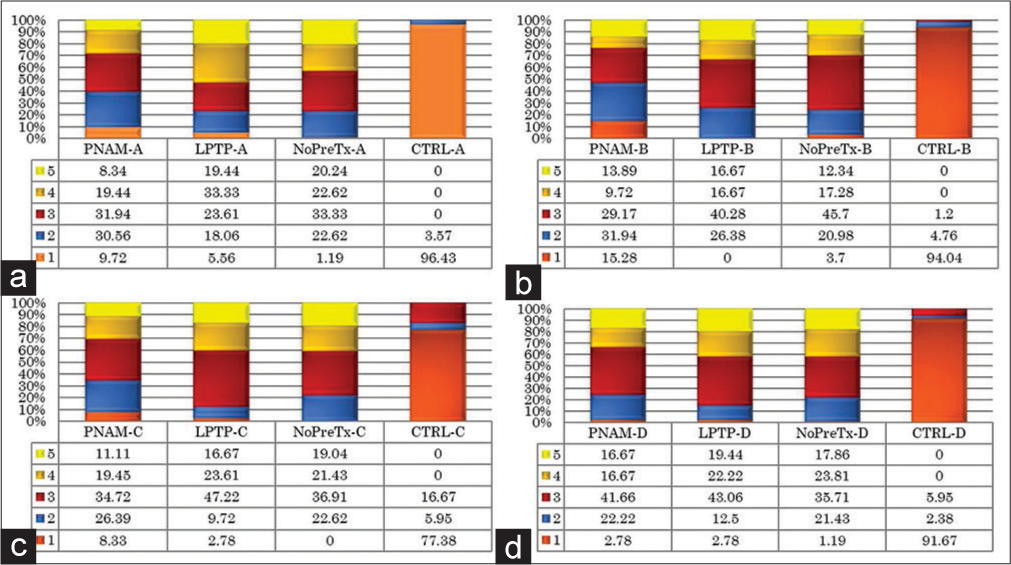
- Frequency distribution charts for nasolabial esthetic parameters with values in percentage (%), (a) nostril form, (b) nasal deviation, (c) nasal form, and (d) vermillion border.
Paired “t”-test of nasolabial esthetic scores for distribution among the groups PNAM, LPTP, NoPreTx, and CTRL was performed [Table 4]. Significant difference exists between PNAM group when compared to LPTP (P = 0.000) and NoPreTx (P = 0.001) for the nasolabial scores given to them by evaluators. Groups LPTP-NoPreTx did not differ significantly in the scoring (P = 0.172). The CTRL group was significantly different from PNAM (P = 0.000), LPTP (P = 0.000), and CTRL (P = 0.000) in terms of nasolabial esthetic scores. Cronbach’s alpha was found close to 0.9 both for individual components scored and for overall score, thus establishing that the scale of measurement and the esthetic evaluation scores was coherent and reliable. Fleiss Kappa statistics showed that the evaluators had a moderate agreement for the nostril form, nasal deviation, and vermillion border scores whereas the evaluators agreed only fairly on nasal deviation scores [Table 5].
| Intergroup comparison | Paired differences | 95% confidence interval | Sig. (2-tailed) | ||
|---|---|---|---|---|---|
| Mean (SD) | Std. Error | Lower | Upper | P-value | |
| PNAM–LPTP | −0.42 (1.43) | 0.08408 | −0.5891 | −0.25812 | 0* |
| PNAM–NoPreTx | −0.29 (1.47) | 0.08691 | −0.46967 | −0.12755 | 0.001* |
| PNAM–CTRL | 1.81 (1.24) | 0.07289 | 1.66209 | 1.94902 | 0* |
| LPTP–NoPreTx | 0.13 (1.55) | 0.09133 | −0.05477 | 0.30477 | 0.172 |
| LPTP–CTRL | 2.23 (1.15) | 0.06752 | 2.09626 | 2.36207 | 0* |
| NoPreTx–CTRL | 2.14 (1.16) | 0.0634 | 2.01517 | 2.26459 | 0* |
| Cronbach’s alphaa | Kappa (κ)b | |
|---|---|---|
| Nostril form (a) | 0.998 | 0.42 |
| Nasal deviation (b) | 0.997 | 0.485 |
| Nasal form (c) | 0.998 | 0.209 |
| Vermillion border (d) | 0.999 | 0.529 |
DISCUSSION
Esthetics is a highly subjective topic and its quantification on a scale varies from professionals to layperson. Studying nasolabial esthetics in cleft infants is even more complex as it poses the effect of numerous uncontrollable variables on the results.
Although there are laser recoded 3D imaging data available already, 2D photographic evaluation is still the most widely used, accessible and cheapest means of recording and reliably reproducing clinical records.[10]
In this study, an excellent coherence (Cronbach’s alpha > 0.9) of the nasolabial esthetic scores and a moderate interevaluator agreement (Fleiss Kappa = 0.50) shows consistence with the previous studies employing Asher-McDade scoring criteria for nasolabial esthetic evaluation.[9,11,12] Nasolabial esthetic scores showed statistically significant difference between the cleft groups and the CTRL group which confirmed findings of the previous studies.[13]
This study showed a significant difference in nasolabial scores between the group which underwent PNAM therapy and the groups which underwent LPTP and/or cheilorhinoplasty. These results concur with findings of the previous studies which report immediate improvement of post-surgical nasal symmetry following NAM therapy.[7,14,15] A previous multicenter study reported the scores in categories of vermillion border, nasolabial frontal, and overall nasolabial esthetics to be significantly better in the center where patient groups underwent PSIO in infancy as compared to the centers where primary surgical repair was performed without PSIO.[16] The results of the present study also were consistent with the previous studies, with outcomes being better for PNAM group. Movement of the infants while capturing the photographic data was controlled to some extent using a head stabilizer pillow and was compensated using fast shutter speeds of the DSLR camera system. Moreover, the nasolabial esthetic method devised by Asher-McDade though is a reliable means of scoring, but does not take into consideration other features of repaired lip such as postsurgical hypertrophic scar, white roll, and philtrum.
CONCLUSION
The unilateral cleft lip and palate infants who turned up early within 1st month of birth to the craniofacial center were lucky enough to take advantage of PNAM therapy and had significantly better results in terms of esthetics as compared to the group of infants who got only LPTP as intervention or NoPreTx before cheilorhinoplasty.
Acknowledgments
We thank the orthodontics faculty Dr. Ronaldo Vergara, Dr. Gary Estomaguio, Dr. Paolo M.B. Manzano, and Dr. Ann L. Querijero for helping to review this study at different stages. We acknowledge the executive director Ms. Mel E. Maranan and other staff at the craniofacial foundation. Our heartfelt gratitude to Dr. M. Samuel Noordhoff and Dr. Eric J.W. Liou for connecting us with the craniofacial foundation. For statistical mentoring, we thank Dr. Fredegusto.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- The development of an index of orthodontic treatment priority. Eur J Orthod. 1989;11:309-32.
- [CrossRef] [PubMed] [Google Scholar]
- Unilateral cleft lip-approach and technique. Semin Plast Surg. 2005;19:313-28.
- [CrossRef] [Google Scholar]
- Nasoalveolar molding for infants born with clefts of the lip, alveolus, and the palate. Semin Plast Surg. 2005;19:294-301.
- [CrossRef] [Google Scholar]
- Presurical nasoalveolar molding therapy for the treatment of unilateral cleft lip and palate: A preliminary study. Cleft Palate Craniofac J. 2007;44:8-12.
- [CrossRef] [PubMed] [Google Scholar]
- Nonsurgical correction of congenital auriculardeformities in the early neonate: A preliminary report. Plast Reconstr Surg. 1984;73:38-51.
- [CrossRef] [PubMed] [Google Scholar]
- Preoperative non-surgical over-correction of cleft lip nasal deformity. Br J Plast Surg. 1991;44:5-11.
- [CrossRef] [PubMed] [Google Scholar]
- Presurgical nasoalveolar molding in infants with cleft lip and palate. Cleft Palate Craniofac J. 1999;36:486-98.
- [CrossRef] [PubMed] [Google Scholar]
- A six-center international study of treatment outcome in patients with clefts of the lip and palate: Part 4. Assessment of nasolabial appearance. Cleft Palate Craniofac J. 1992;29:409-12.
- [CrossRef] [PubMed] [Google Scholar]
- Quantitative 3D soft tissue analysis of symmetry prior to and after unilateral cleft lip repair compared with non-cleft persons (performed in Cambodia) J Craniomaxillofac Surg. 2008;36:431-8.
- [CrossRef] [PubMed] [Google Scholar]
- Cleft lip and palate care in the United Kingdom--the clinical standards advisory group (CSAG) study. Part 2: Dentofacial outcomes and patient satisfaction. Cleft Palate Craniofac J. 2001;38:24-9.
- [CrossRef] [PubMed] [Google Scholar]
- Craniofacial development in children with unilateral clefts of the lip, alveolus, and palate treated according to four different regimes. I. Maxillary development. Scand J Plast Reconstr Surg Hand Surg. 1991;25:259-67.
- [CrossRef] [PubMed] [Google Scholar]
- Nasolabial symmetry and esthetics in children with complete unilateral cleft lip and palate. Br J Oral Maxillofac Surg. 2012;50:621-5.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term effects of nasoalveolar molding on three-dimensional nasal shape in unilateral clefts. Cleft Palate Craniofac J. 1999;36:391-7.
- [CrossRef] [PubMed] [Google Scholar]
- The progressive changes of nasal symmetry and growth after nasoalveolar molding: A three-year follow-up study. Plast Reconstr Surg. 2004;114:858-64.
- [CrossRef] [PubMed] [Google Scholar]
- Burden of care Analysis of Various Infant Orthopedic Protocols for Improvement of Nasolabial Esthetics in Patients with Complete Unilateral Cleft Lip and Palate. [Dissertation] Toronto, Canada: University of Toronto; 2012.
- [Google Scholar]






