Analysis of the changes in components of smile after maxillary arch distalization using infra-zygomatic crest (IZC) screws – A cephalometric and photographic study

*Corresponding author: Syeda Fathimuz Zahara, Department of Orthodontics, Yenepoya Dental College, Mangaluru, Karnataka, India. Email: syedazahra2@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Zahara SF, Husain A, Khan FA. Analysis of the changes in components of smile after maxillary arch distalization using nfra-zygomatic crest (IZC) screws – A cephalometric and photographic study. J Global Oral Health. 2024;7:39-45. doi: 10.25259/JGOH_21_2022
Abstract
Objectives:
The purpose of this study was to analyze the effects of infra-zygomatic crest (IZC) screws on smile components after maxillary arch distalization.
Materials and Methods:
The study was conducted on 20 subjects (11 boys and 9 girls) between 19 and 30 years. It was a time-bound study where screening of patients was done based on the inclusion and exclusion criteria for a year. Before placement of orthodontic bone screws (IZC), pre-treatment (T0) photographs, and cephalograms were taken where photographs were analyzed using Makhter’s software. After 6–8 months, post-distalization treatment (T1) photographs and cephalograms were taken and evaluated.
Results:
Descriptive statistics were used to obtain the mean and standard deviation for continuous data. Paired t-test was performed to analyze the changes in pre- and post-distalization. The categorical data were calculated using the McNemar test. Differences were considered significant if P < 0.05. Inner commissure right and left, smile arc, posterior maxillary dentition visible - left (PMDVL), upper incisal visibility, and gingival showed statistical significance.
Conclusion:
Maxillary arch distalization using IZC screws was associated with changes in horizontal smile components but mainly in vertical components, reducing the gummy smile, and making the smile esthetically pleasing.
Keywords
Makhter software
Smile
Infra-zygomatic crest (IZC) screws
Class II malocclusion
Distalization
INTRODUCTION
Class II malocclusions are characterized by a mesial relationship of the maxillary arch to the mandibular arch and are frequently seen in orthodontic practice. The cause could be due to skeletal or dental factors or a combination of the two. In patients with Class II division one malocclusion and mild skeletal maxillary excess distalization of the entire maxillary dentition can be a camouflage treatment.[1]
The smile plays an important part in orthodontic diagnosis and treatment planning.[2] Smile is of two types according to Ackerman and Ackerman[3] which are “posed smile” and “unposed smile.” Studies show that an unstrained posed smile is the best smile for recording and analyzing in orthodontics and other fields of dentistry.[4,5] Semi-quantitative method of a smile is analyzed using a photograph.[6]
The distalization of the maxillary molar is of significant value for the treatment of Class II molar relationship associated with normal mandible and acceptable profile.[7] Absolute anchorage systems help in converting borderline surgical cases, into non-surgical, extraction into non-extraction cases, and brings about the esthetic impact which was easily achieved, unlike conventional mechanics.[8]
With the advent of the orthodontic bone screws (OBS), recently, an apt balance was achieved which not only had an extraradicular site of placement in the infra-zygomatic crest (IZC) of the maxilla, with significantly fewer failure rates than regular mini-implants and also does not require extensive surgical intervention for their placement.[9,10]
MATERIALS AND METHODS
The study was conducted on 20 subjects (11 boys and 9 girls) between the age group of 19 and 30 years, who were reported to the Department of Orthodontics and Dentofacial Orthopedics, Yenepoya Dental College. Ethical clearance was obtained from the Ethical Committee (YEC-2) with ethical clearance number YEC 2/198 on January 6, 2020, before the onset of the study. It was a time -bound study where screening of patients was done based on the patient selection between 19 and 30 years with skeletal and dental class II molar relation, no history of orthodontic treatment, overjet of more than 5mm and healthy gingival tissue as inclusion criteria. The patients with no gross facial asymmetry and deformities, systemic disorders, immunocompromised, uncooperative, cleft lip and palate were excluded.
Informed consent was obtained. Photographic records of participants were made using a high-definition camera (Camera-Nikon D3400) with a macro lens (sigma 200 mmf/2.8 macro lens, Japan) and ring flash using AKHTER’s digital setup [Figure 1]. Standardization was done by calibrating the ends of square stickers, in both X- and Y- axis as 10 mm using the MAKHTER facial analysis software (FAS). This sticker was fixed on the patient’s forehead before the smile was captured [Figure 2]. The photographs were analyzed to evaluate the parameters as follows in predicting the smile esthetics. Analysis of the smile was done using MAKHTER FAS. The analysis begins with marking the two ruler points 1 and 2, used for standardization, on the lower and upper border of the square sticker placed on the subject’s forehead. Before placement of OBS IZC, pre-treatment (T0) photographs and cephalograms were taken where photographs repeated. After 6–8 months, post-distalization treatment (T1) photographs and cephalograms were taken and evaluated for the variables as shown in Figures 3 and 4.

- Akhter’s digital setup.

- Photograph with 1 cm square sticker for standardization.
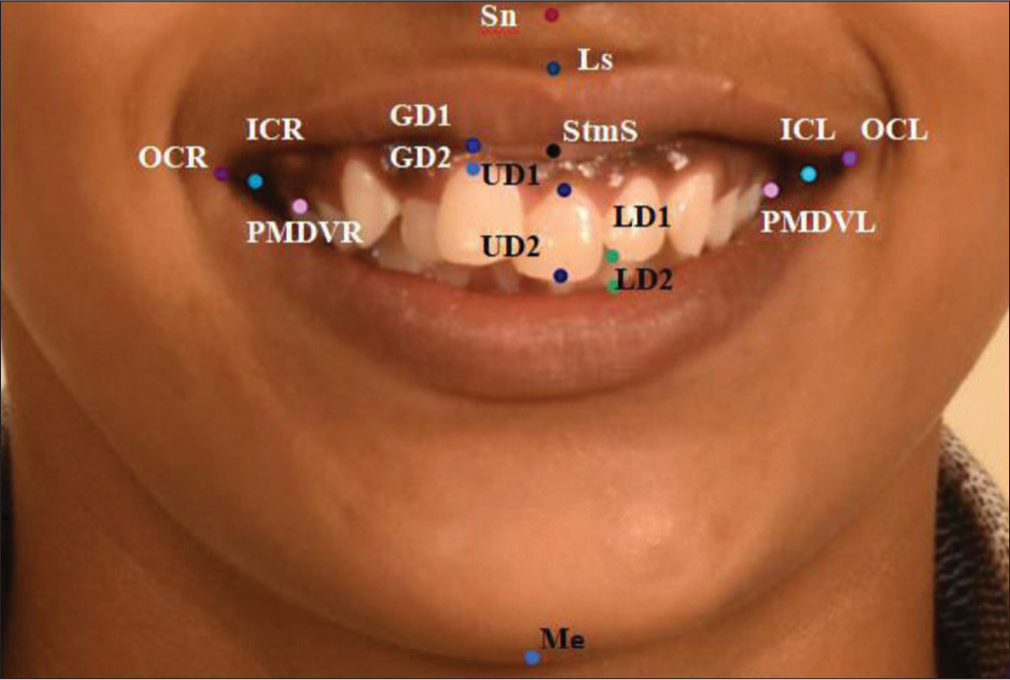
- Landmarks showing in Red-Sn- Subnasale, Light Purple-Ls- Labrale superioris, Pink-PMDVR- Posterior maxillary dentition visible right and PMDVL- Posterior maxillary dentition visible left, Blue-ICR- Inner commissure right & ICL- Inner commissure left, Violet-OCR- Outer commissure right and OCL- Outer commissure left, Light violet, Black-StmS, Light Violet-GD- Gingival display-GD1 and GD2, Purple-UD1 and UD2-UD- Upper incisal display, Green-LD1 & LD2-LD- Lower incisal display, Dark violet- MeMenton.

- Cephalometric parameters showing skeletal parameters, (.) a. SNA, ( .) b. SNB, and ( .) c. ANB, dental parameters, (.) a. Upper incisor to SN, (.) b. Upper incisor to NA(angle), ( .) c. Upper incisor to NA(linear), and (.) d. Upper incisor to NF. Soft-tissue parameters, and (.) a. Nasolabial angle and ( .) b. Upper lip to S –line. All 1 as red dots, 2 as blue dots, 3 as green dots.
Continuous variables
Horizontal parameters
Outer commissure width – Distance between outer commissure of the right and left side
Inner commissure width – Distance between inner commissure of the right and left side
Width of posterior maxillary dentition visible – Distance between posterior maxillary dentition visible on the right and left side
Buccal corridor width right side – Distance between inner commissure and posterior maxillary dentition visible on the right side
Buccal corridor width left side – Distance between inner commissure and posterior maxillary dentition visible on the left side.
Vertical parameters
Philtrum height – Distance between subnasale and labrale superior
Upper lip thickness – Distance between labrale superior and stomion superior
Lower anterior facial height – Distance between subnasale and menton
Upper incisal visibility – Amount of the upper incisal exposure on the smile
Lower incisal visibility – The amount of the lower incisal exposure on the smile
Gingival show – Amount of gingival display of the upper central incisors from marginal gingival to the inferior border of the upper lip on the smile.
Dichotome variables
Smile arc – Consonant or non-consonant
Lip line – High or low
Smile symmetry – Assessed by the parallelism of the commissural and pupillary lines.
Lateral cephalograms of pre- and post-distalization were assessed using the following parameters assessed in lateral cephalograms which are as follows [Figure 4];
-
Skeletal parameters
Angle between Sella, Nasion and subspinale point A (SNA)
Angle between Sella, Nasion and Subspinale point B (SNB)
Angle formed by point A, Nasion and point B (ANB)
-
Dental parameters
Upper incisor to Nasion to point A (NA)
Upper incisor to Nasal floor (NF)
Upper incisor to Sella -Nasion (SN)
-
Soft-tissue parameters
Upper lip to S-line
Nasolabial angle
The data were analyzed using SPSS software version IBM SPSS Statistics for Windows software (version 23 IBM Corp., Armonk, NY) at a 5% level of significance. The descriptive statistics were used to obtain the mean and standard deviation (SD) for continuous data. Paired t-test was performed to analyze the changes in pre- and post-distalization. The data are shown as mean (SD) with a 95% confidence interval. The categorical data were calculated using the McNemar test. Differences were considered significant if the probability was <0.05 (i.e., P < 0.05).
RESULTS
The comparison of horizontal parameters among pre- and post-distalization in the orthodontic treatment group shows that the average outer commissure right and left did not change significantly after the distalization. The same conclusion holds for all the variables mentioned except, for the inner commissure right and left (ICR-ICL) variable, where the mean was found to be higher after distalization. The paired sample t-test was used to check whether the average changed significantly after the distalization. The mean difference was found to be not statistically significant (P < 0.05) between other variables measured, as shown in Table 1. The comparison of vertical smile component variables among pre- and post-distalization in the orthodontic treatment group shows that all P values are more than 0.05 indicating an insignificant change (no change), as shown in Table 2. The paired sample t-test is used to compare the averages before and after the distalization. The proportion of non-consonant smile arcs after distalization decreased significantly from 60% to 10%, as shown in Graph 1. The mean difference was found to be statistically significant (P < 0.05), as shown in Graph 2. Comparison of cephalometric soft-tissue parameters pre- and post-distalization shows improved nasolabial angle, as shown in Table 3 and Graph 3.
| Mean | n | SD | Std. error mean | t | P-value | 95% CI | ||
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| OCR-OCL | ||||||||
| Pre | 6.6240 | 20 | 0.74347 | 0.16625 | −0.384 | 0.705 | −0.27096 | 0.18696 |
| Post | 6.6660 | 20 | 0.71450 | 0.15977 | ||||
| ICR-ICL | ||||||||
| Pre | 5.9560 | 20 | 0.67336 | 0.15057 | −2.178 | 0.042 | −0.42745 | −0.00855 |
| Post | 6.1740 | 20 | 0.57838 | 0.12933 | ||||
| PMDV-PMDVL | ||||||||
| Pre | 5.3120 | 20 | 0.62303 | 0.13931 | −0.697 | 0.494 | −0.34636 | 0.17336 |
| Post | 5.3985 | 20 | 0.57327 | 0.12819 | ||||
| ICR-PMDVR | ||||||||
| Pre | 0.3640 | 20 | 0.13100 | 0.02929 | −0.074 | 0.942 | −0.05846 | 0.05446 |
| Post | 0.3660 | 20 | 0.12878 | 0.02880 | ||||
| ICL-PMDVL | ||||||||
| Pre | 0.3190 | 20 | 0.10745 | 0.02403 | −0.281 | 0.782 | −0.07177 | 0.05477 |
| Post | 0.3275 | 20 | 0.07383 | 0.01651 | ||||
Statistical test: Paired t-test, Level of significance: P<0.05. CI: Confidence interval, SD: Standard deviation. OCR-OCL: Outer commissure width, ICR-ICL: Inner commissure width, PMDV-PMDVL: Posterior maxillary dentition visible, ICR-PMDVR: Buccal corridor width–right, ICL-PMDVL: Buccal corridor width–left, n- Number of subjects, Pre: Pre-distalization, Post: Post-distalization
| Mean | n | SD | Std. error mean | t | P-value | 95% CI | ||
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Sn-LS | ||||||||
| Pre | 0.8475 | 20 | 0.21280 | 0.04758 | 1.389 | 0.181 | −0.02481 | 0.12281 |
| Post | 0.7985 | 20 | 0.29518 | 0.06600 | ||||
| LS-StmS | ||||||||
| Pre | 0.6635 | 20 | 0.16187 | 0.03620 | 0.243 | 0.810 | −0.04944 | 0.06244 |
| Post | 0.6570 | 20 | 0.21873 | 0.04891 | ||||
| Sn-Me | ||||||||
| Pre | 6.9175 | 20 | 0.67571 | 0.15109 | −0.044 | 0.965 | −0.19364 | 0.18564 |
| Post | 6.9215 | 20 | 0.57212 | 0.12793 | ||||
| UD1-UD2 | ||||||||
| Pre | 0.8855 | 20 | 0.24094 | 0.05388 | −1.602 | 0.126 | −0.13030 | 0.01730 |
| Post | 0.8290 | 20 | 0.17179 | 0.03841 | ||||
| LD1-LD2 | ||||||||
| Pre | 0.2110 | 20 | 0.20269 | 0.04532 | −0.019 | 0.985 | −0.11308 | 0.11108 |
| Post | 0.2120 | 20 | 0.15109 | 0.03378 | ||||
| GD1-GD2 | ||||||||
| Pre | 0.0765 | 20 | 0.18259 | 0.04083 | 0.210 | 0.836 | −0.06288 | 0.07688 |
| Post | 0.0695 | 20 | 0.13113 | 0.02932 | ||||
Statistical test: Paired t-test, Level of significance: P < 0.05. CI: Confidence interval, SD: Standard deviation. Sn-Ls: Philtrum height, LS-StmS: Upper lip thickness, Sn-Me: Lower anterior facial height, UD1-UD2: Upper incisal visibility, LD1-LD2: Lower incisal visibility, GD1-GD2: Gingival show, n- Number of subjects

- Comparison of the mean (standard deviation) of smile arc pre- and post-distalization. Green indicates mean of smile arc pre- distalization and Red indicates increased mean post- distalization.

- Comparison of the mean (standard deviation) of smile attractiveness pre- and post-distalization using Visual Analogue Scale (VAS).
| Mean | n | SD | Std. error mean | t | P-value | 95% CI | ||
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| SNA | ||||||||
| Pre | 83.100 | 20 | 1.7741 | 0.3967 | 15.387 | 0.021 | 1.5552 | 2.0448 |
| Post | 81.300 | 20 | 1.4546 | 0.3253 | ||||
| SNB | ||||||||
| Pre | 77.400 | 20 | 2.1374 | 0.4779 | −8.794 | 0.012 | −2.1046 | −1.2954 |
| Post | 79.100 | 20 | 1.8610 | 0.4161 | ||||
| ANB | ||||||||
| Pre | 5.550 | 20 | 0.8256 | 0.1846 | 22.465 | 0.013 | 2.9925 | 3.6075 |
| Post | 2.250 | 20 | 0.7864 | 0.1758 | ||||
| UI to NA (linear mm) | ||||||||
| Pre | 8.750 | 20 | 1.2927 | 0.2891 | 15.657 | 0.021 | 3.9851 | 5.2149 |
| Post | 4.150 | 20 | 0.3663 | 0.0819 | ||||
| UI to NA degree | ||||||||
| Pre | 35.400 | 20 | 2.2572 | 0.5047 | 20.739 | 0.023 | 11.1935 | 13.7065 |
| Post | 22.950 | 20 | 3.4561 | 0.7728 | ||||
| LAFH (mm) | ||||||||
| Pre | 76.100 | 20 | 2.0235 | 0.4525 | 27.606 | 0.011 | 1.7559 | 2.0441 |
| Post | 74.200 | 20 | 2.0157 | 0.4507 | ||||
| UI to NF (mm) | ||||||||
| Pre | 32.400 | 20 | 1.6026 | 0.3584 | 7.346 | 0.012 | 1.5374 | 2.7626 |
| Post | 30.250 | 20 | 1.0195 | 0.2280 | ||||
| UI to SN (angle) | ||||||||
| Pre | 123.650 | 20 | 5.3732 | 1.2015 | 21.443 | 0.010 | 9.9263 | 12.0737 |
| Post | 112.650 | 20 | 6.8231 | 1.5257 | ||||
| Nasolabial angle | ||||||||
| Pre | 101.950 | 20 | 5.9513 | 1.3308 | −1.238 | 0.032 | −182.7208 | 46.9208 |
| Post | 169.850 | 20 | 244.4690 | 54.6649 | ||||
| Upper lip to S-line (mm) | ||||||||
| Pre | 3.700 | 20 | 0.7327 | 0.1638 | 11.414 | 0.023 | 1.9599 | 2.8401 |
| Post | 1.300 | 20 | 0.8013 | 0.1792 | ||||
Statistical test: Paired t-test, Level of significance: P<0.05. CI: Confidence interval, SD: Standard deviation. LAFH: Lower anterior facial height, SNA: Sella Nasion Point A angle, SNB: Sella Nasion Point B angle, ANB: SNA minus SNB, UI to NA: Upper insisor to nasion Point A

- Comparison of cephalometric soft-tissue parameters pre- and post-distalization.
DISCUSSION
Class II malocclusion with maxillary arch distalization is treated since the 19th century using headgear[11-13] and later numerous removable and fixed appliances emerged to provide easier action when placed intraorally. With the advent of bone screws, increased anchorage and improved smile were the advantages.[14]
The beauty or attractiveness of a person is a perception that is subjective and changes with a person’s feelings, beliefs, and desires.[15] The variation in smile could be due to the camera setup used. To improve a smile design, it is necessary to record a “posed smile” as an intentional, non-pressure, static, natural, and reproducible smile.[16] Numerous studies were done using various setups to capture the smile, but, in our study, Makhter’s setup[17] is used to achieve the best-posed smile for the frontal photographs to analyze the smile components.
A study done by Maganzini et al.,[18] reported that commissural width increases significantly with orthodontic treatment and contributes to improving smile esthetics. Among the horizontal parameters measured, our study showed an increase in commissure width after distalization which was contributing to an improvement in smile esthetics. Studies by Sarver[19] and Dierkes[20] reported that it is important to reach proper buccal corridor dimensions to increase smile esthetics. Our study showed that the mean buccal corridor width was found to be less after distalization. Vertical parameters did not show much significant difference in our study, but the mean was found to be higher after distalization in parameters such as lower anterior facial height and upper incisal visibility. The increased mean of lower anterior facial height indicates that distalization can improve lower anterior facial height.
In a study conducted by Lauria et al.,[21] the most attractive smile according to the observers was the smile that exposed upper central incisors and a small band of the gingiva. The vertical parameters such as philtrum height and upper lip thickness all show decreased mean after distalization. These findings indicate that distalization does not show any improvement in lip thickness and philtrum height. Among dichotome variables, the smile arc shows a statistically significant difference before and after distalization. Other variables such as lip line and smile symmetry did not show any statistically significant difference. A smile arc is described as a consonant if it follows the curvature of the lower lip and a non-consonant if it is not parallel to the lower lip.[4]
In general, the lip line is optimal when the upper lip reaches the gingival margin, displaying the total cervicofacial length of the maxillary central incisors, along with the interproximal gingiva. Because female lip lines are an average of 1.5 mm higher than male lip lines, 1–2 mm of gingival display at maximum smile could be considered normal for females.[4] In the present study, the lip line shows improvement after distalization.
In this study, comparisons of smiles and attractiveness were done using a visual analog scale. The mean difference was found to be statistically significant (P < 0.05) post-distalization. This study shows that smile attractiveness is improved after distalization. A smile line that displays the entire length of the teeth and some gingival tissue is associated with youth. In contrast, a smile line with only a portion of the teeth visible results in a less youthful and unaesthetic smile.[22]
According to Batwa et al., facial types do not influence smile esthetics.[23] However, our study showed brachycephalic facial types to have improved horizontal parameter inner commissure width. On the cephalometric assessment, soft-tissue components showed statistically significant improvement which could be a contributing factor to the smile components. Furthermore, it was found that there were significant changes in both skeletal and dental components. In our study, the mean was found to be higher after distalization among parameters such as commissure width, posterior maxillary dentition visibility, lower anterior facial height, and upper incisal visibility indicating that these factors can improve the smile esthetics. Among dichotome variables, the smile arc shows a statistically significant difference after distalization. Lip line and Smile symmetry did not show any statistically significant difference. The mean was found to be higher after distalization among all three parameters indicating that these variables can contribute to smile esthetics. Smile attractiveness evaluated by the visual analog scale shows a higher mean after aligning and decrowding indicating that smile attractiveness is improved after distalization.
Limitations of the study
It is a two-dimensional study and further three-dimensional would help in a better evaluation
The sample size is inadequate to decide on the proper evaluation of smile components
Further studies need to be done to compare the effectiveness of IZC bone screws with the mini-implants placed at the infra-zygomatic crest area.
As very less literature is available based on facial types further studies need to be done.
CONCLUSION
Overall, there was a statistically significant change in horizontal parameters in smile components in the ICRICL (Inner commissure width) post-distalization and a clinically significant change in vertical smile components
Among the females, horizontal parameters in smile components in the ICR-ICL (Inner commissure width) and posterior maxillary dentition visible-PMDVL and vertical parameter upper incisal visibility: UD1–UD2 showed significant improvement post-distalization. Among males, no significant changes were noted post-distalization
Among the facial types evaluated, only the brachyfacial type showed improvement in horizontal parameter, ICRICL (Inner commissure width) post-distalization
There was a change in soft-tissue components cephalometrically which corelate to the change in smile components
Among the dichotome variables assessed, smile arc has shown to be significantly improved post-distalization
The visual analog scale was rated to be more among layman and undergraduates when compared to others post-distalization
Hence, maxillary arch distalization using IZC screws was associated with changes in smile components mainly in vertical parameters, thereby reducing the gummy smile and making the smile esthetically pleasing.
Ethical Approval
Ethical clearance was obtained from the Ethical Committee (YEC-2) with ethical clearance number YEC 2/198 on January 6, 2020
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI
Financial support and sponsorship
Nil.
References
- Comparative evaluation of displacement and stress distribution pattern during maxillary arch distalization with Infra Zygomatic Screw-A three-dimensional finite element study. Int Orthod. 2021;19:291-300.
- [CrossRef] [PubMed] [Google Scholar]
- Smile attractiveness. Self-perception and influence on personality. Angle Orthod. 2007;77:759-65.
- [CrossRef] [PubMed] [Google Scholar]
- Five-year experience with orthodontic miniscrew implants: A retrospective investigation of factors influencing success rates. Am J Orthod Dentofacial Orthop. 2009;136:158.e1-10. discussion 158-9
- [CrossRef] [PubMed] [Google Scholar]
- Laypeople's perceptions of frontal smile esthetics: A systematic review. Am J Orthod Dentofacial Orthop. 2016;150:740-50.
- [CrossRef] [PubMed] [Google Scholar]
- Maxillary molar distalization with the first class appliance. BMJ Case Rep. 2014;2014:bcr2013200182.
- [CrossRef] [PubMed] [Google Scholar]
- An Investigation of Orthodontic Miniscrew Implant Success. In: Phuket. 5th World Implant Orthodontic Conference. 2023.
- [Google Scholar]
- Acceptance of orthodontic miniscrews as temporary anchorage devices. Patient Prefer Adherence. 2014;8:933-7.
- [CrossRef] [PubMed] [Google Scholar]
- Mini-screw or mini-plate, which is better for whole upper arch distalization. News Trends Orthod. 2007;1:1-2.
- [Google Scholar]
- Adenoid Growths, Mouth Breathing and Thumb-Sucking in Their Relation to Deformities of the Jaws and Irregular Teeth Vol Vol 34. Maharashtra: Dental Cosmos; 1892. p. :16. 100, 357, 442
- [Google Scholar]
- Extraoral force-facts and fallacies. Am J Orthod Dentofacial Orthop. 1955;41:490-505.
- [CrossRef] [Google Scholar]
- Biomechanics for correction of vertical skeletal Class II and dental Class II subdivision malocclusion using infrazygomatic screws. IJMSIR. 2020;5:111-7.
- [Google Scholar]
- The role of the golden proportion in the evaluation of facial esthetics. Angle Orthod. 2013;83:801-8.
- [CrossRef] [PubMed] [Google Scholar]
- Three-camera setup to record simultaneously standardized high-definition video for a smile analysis. Am J Orthod Dentofacial Orthop. 2017;152:711-6.
- [CrossRef] [PubMed] [Google Scholar]
- Improvement in smile esthetics following orthodontic treatment: A retrospective study utilizing standardized smile analysis. Angle Orthod. 2014;84:492-9.
- [CrossRef] [PubMed] [Google Scholar]
- The importance of incisor positioning in the esthetic smile: The smile arc. Am J Orthod Dentofacial Orthop. 2001;120:98-111.
- [CrossRef] [PubMed] [Google Scholar]
- The beauty of the face: An orthodontic perspective. J Am Dent Assoc. 1987;115:89E-95.
- [CrossRef] [PubMed] [Google Scholar]
- Perception of oral and maxillofacial surgeons, orthodontists, and laypersons in relation to the harmony of the smile. J Craniomaxillofac Surg. 2014;42:1664-8.
- [CrossRef] [PubMed] [Google Scholar]
- The maxillary sagittal appliance: A clinical study. Am J Orthod Dentofacial Orthop. 1987;91:271-85.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of the smile on the perceived facial type esthetics. Biomed Res Int 2018
- [CrossRef] [PubMed] [Google Scholar]







