Translate this page into:
Comparison of perception of pain following orthodontic extraction with oral analgesics over adjuvant herbal patch

*Corresponding author: Dr. Aparna Sukumaran, Department of Public Health Dentistry, Ragas Dental College and Hospital, 2/102, East Coast Road, Uthandi, Chennai - 600 119, Tamil Nadu, India. abi_aparna1986@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Sukumaran A, Fiona RJ, Monisha B, Zulkifli N, Vijayarangan S, Kumar PD. Comparison of perception of pain following orthodontic extraction with oral analgesics over adjuvant herbal patch. J Global Oral Health 2020;3(1):18-22.
Abstract
Objectives:
Pain that follows extraction of any tooth is an acute, short-lasting (2 h–3 days) pain that reaches its maximum intensity during the early (first 4 h) post-extraction period (Kaur et al., 2016). Pain management postoperatively is essential as it helps to minimize discomfort to the patient, reducing the risk of infection, speeding the recovery period. Although several methods have been used for pain management, no study has been conducted on the efficacy of herbal patch as pain relief method in dental extractions. This present study was conducted to evaluate the effectiveness of herbal patch along with oral analgesics in controlling the post- extraction pain compared to routine oral analgesics alone.
Materials and Methods:
An interventional study was conducted among 30 orthodontic patients aged 13–25 years. Written consent and ethical clearance were obtained. A split-mouth design was used with herbal patch and oral analgesic for post-extraction pain management for the study participants. Visual analog scale was used to assess the pain post-extraction at 4, 8, 12, 16, 20, and 24 h of the 1st day. Data collected were subjected to appropriate statistical test using SPSS version 20.
Results:
A highly statistical difference was seen between the two groups and within the groups (P < 0.001).
Conclusion:
Transdermal herbal patch seems to be a promising analgesic modality for the management of mild- to-moderate pain following dental extractions.
Keywords
Herbal patch
Post-extraction pain
Orthodontic patients
INTRODUCTION
According to the WHO, pain is defined as “unpleasant sensory or emotional experience associated with actual or potential tissue damage.” The pain that follows extraction of any tooth is an acute, short-lasting (2 h–3 days) pain that reaches its maximum intensity during the early (first 4 h) post-extraction period.[1] Pain management postoperatively is essential as it helps to minimize discomfort to the patient, reducing the risk of infection, speeding the recovery period. Hence, the success of a dental treatment is not only determined by the appropriate operative technique but also includes prevention and management of post-operative complications.
The contribution of oral nonsteroidal anti-inflammatory drugs (NSAIDs) in the mitigation of pain following extraction cannot be underestimated. NSAIDs are one of the most common analgesics that are being used by dentists to help relieve pain and distress after extraction.
However, the adverse effect of taking NSAID orally imposes a complication and discomfort to some patients. This includes irritation to the gastrointestinal system due to its high plasma concentration, reduced concentration systemically available due to the first-pass metabolism. Hence, to reduce such occurrences, innovative method of drug delivery has been explored.
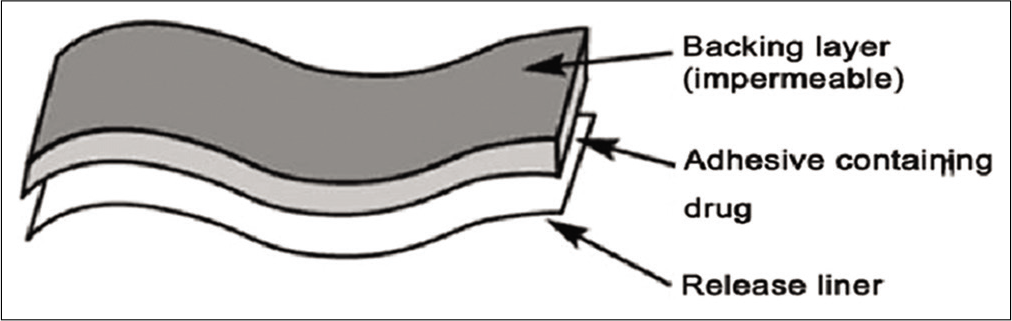
Transdermal drug delivery, a type of local drug delivery system offers non-invasive delivery of medications through the skin surface. They are defined as “medicated adhesive patch which is placed above the skin to deliver a specific dose of medication through the skin with a predetermined rate of release to reach into the bloodstream [Figure 1].”[2] This route of administration differs from the traditional topical administration in that, after penetration of the skin barrier, the drug enters the circulation to be distributed systemically. The major advantage is that it bypasses the first- pass hepatic metabolism providing enhanced bioavailability. Furthermore, it offers controlled absorption, thus avoiding any gastrointestinal medication-related side effects. Patient compliance is improved as patches are simple, non-invasive, and convenient.
- Matrix controlled transdermal patch system.
However, during recent years, people are inclined to use herbal medicines due to their lower complications and fewer side effects than synthetic drugs. The use of herbal medicine with its therapeutic properties in pain management is not new as it has been used since ancient times and has been explored since. They have also been manufactured as transdermal herbal patch by combining the Ayurvedic tradition and modern science by incorporating active ingredients such as menthol which helps in alleviating pain by its counterirritant effect. According to gate control theory, menthol elicits an analgesic effect by activating Transient Receptor Potential Melastatin 8 (TRPM8) channels located on sensory nerves and on C and Aδ nociceptors to reduce pain transmission.[3] While these topically applied agents are effective at reducing perceived pain from various musculoskeletal injuries, they may also have other non-specific effects on neural and vascular tissues containing TRPM8 receptors.[3] In addition, menthol activates gamma-aminobutyric acid and blocks voltage-gated sodium and calcium channels in the dorsal horn and preferentially binds to inactivated channels, producing a central analgesic effect.[4] Hence, even though the herbal patch is placed away from the extraction site, it may modulate the extraction pain, thus providing relief.
Till date, no studies have been conducted on the efficacy of herbal patch as pain relief method in dental extractions. Thus, this present study was conducted to evaluate the effectiveness of herbal patch along with oral analgesics in controlling the post-extraction pain compared to routine oral analgesics alone.
MATERIALS AND METHODS
The ethical clearance for the study was provided by the Institutional Review Board, of the teaching dental institution and all subjects were informed about the nature of the study and probable side effects from the drugs being administered. A written informed consent from all subjects as well as parental consent was obtained as some of the subjects were below the age of 18 years old.
A total of 30 young orthodontic patients requiring non-surgical extraction of bilateral maxillary and mandibular first premolar were selected for this study. Armamentarium used for extraction procedure is provided in Figure 2. The study involved a split-mouth technique. The subjects belonged to both sexes and were within the age range of 13–25 years old. In the pre- operative visit, the patients were examined and investigated appropriately. All the subjects for the study had a healthy periodontal status and none of their teeth had extensive decay. Subjects with history or clinical evidence of allergy to NSAIDs or those with any ulceration or medication within the past 6 months were excluded from the sample. Subjects with a history of systemic disease such as bronchial asthma, epilepsy, and emotional and psychosomatic disorders were also excluded from the study. Non-surgical extraction (closed method of extraction) was done of the particular tooth on the day of the appointment of the subjects. A time limit of 30 min was given for each patient; any procedure involving any other method other than the standard closed method of extraction or extension of the proposed duration of the procedure were excluded from the study.

- Materials used for extraction.
The right maxillary and mandibular first premolar were first extracted successively in the same appointment using a standardized armamentarium, given prescribed routine antibiotics and analgesics, i.e., Tab. aceclofenac 200 mg (Acelase-SR) thrice daily for 3 days and antibiotic, i.e., Tab. amoxicillin 500 mg. The standard post-extraction instructions were given, and the patients were given helpline numbers to contact in case of emergency.
The pain intensity following non-surgical extraction was assessed using a visual analog scale (VAS). Patients were given a score number between 0 and 10, 0 representing no pain and 10 demonstrating the worst conceivable pain. Pain severity was assessed on the 1st postoperative day at 4, 8, 12, 16, 20, and 24 h. Prescribed medication was continued to be taken for the next 2 post-operative days.
Tramadol 500 mg tablets were permitted to be used as rescue medication and a total of nine tablets were provided to each of the patients for the 3 post-operative days. The patients were asked to maintain a record of the number of tramadol tablets consumed on the pain assessment charts and to return the remaining tablets to operator on their next visit.
After 3 post-operative days, a period of 1 week was given to allow for the complete washout of drug from the body and the patients were recalled.
The left maxillary and mandibular first premolars were then extracted and prescribed routine medications (Tab. aceclofenac 200 mg-Acelase-SR thrice daily for 3 post- operative days and antibiotic 500 mg amoxicillin given based on the study case) along with herbal transdermal patch (Relyon PAS+, active 12 h) Figure 3 that was given twice daily for 3 days. On each of the following 12 h, the patch was changed and a new one placed, thus placing a total of six patches over the 3 post-operative days. The subjects were asked to report the intensity of pain as mentioned above on the 1st post-operative day. The subsequent 2 days, prescribed medication is continued along with the herbal transdermal patch. The patients were permitted to use Tramadol 500 mg tablets as rescue medication during the post-operative period. All the subjects were properly explained regarding the application of the transdermal patch before discharging.

- Represents the cover of herbal transdermal patch (Relyon PAS+).
The patches were applied on a clean hairless area on the left or right shoulders which were subsequently replaced the next 12 h to another area of application to avoid contact dermatitis in the area of application.
At the end of the study, only 25 patients reported back with the VAS and recorded data obtained were statistically evaluated.
Statistical analysis
Data were entered into Microsoft Excel sheet 2010 and we subjected appropriate test using SPSS software version. 20.0. Normality of the data was assessed using Kolmogorov test.
As the data were heterogeneous, Mann-Whitney U-test was used for between-group comparison and Friedman with Wilcoxon Bonferroni correction was used for within-group comparison. The level of significance was fixed at 0.05.
RESULTS
Fifty participants were subjected to two different interventions (oral and oral analgesic and patch) with a window period of 1 week. Table 1 represents the post-operative pain score between the two interventions statistically evaluated.
| Group | Duration | Right | Left | Z value | P value | |
|---|---|---|---|---|---|---|
| 1 (oral analgesics) | 2 (oral analgesic and transdermal patch) | 4 h | 8.16 | 7.80 | −6.485 | 0.000* |
| 8 h | 6.44 | 5.48 | −6.286 | 0.000* | ||
| 12 h | 5.46 | 3.48 | −6.135 | 0.000* | ||
| 16 h | 5.46 | 1.28 | −6.135 | 0.000* | ||
| 20 h | 2.74 | 2.72 | −6.595 | 0.000* | ||
| 24 h | 1.62 | 4.88 | −6.701 | 0.000* |
Mann–Whitney U-test – Significant level P≤0.05*
A within-group comparison showed a high statistically significant difference within different time intervals in both groups except in Group A – time period between 12 and 16 h was not statistically significant as seen in Table 2.
| Groups | Time points | P value | Time points | Adjusted P value |
|---|---|---|---|---|
| Group A oral | 4 h–8 h | <0.001* | 4 h–8 h | <0.001# |
| 8 h–12 h | 8 h–12 h | <0.001# | ||
| 12 h–16 h | 12 h–16 h | 1.000 | ||
| 16 h–20 h | 16 h–20 h | <0.001# | ||
| 20 h–24 h | 20 h–24 h | <0.001# | ||
| Group 2 oral+Patch | 4 h–8 h | <0.001* | 4 h–8 h | <0.001# |
| 8 h–12 h | 8 h–12 h | <0.001# | ||
| 12 h–16 h | 12 h–16 h | <0.001# | ||
| 16 h–20 h | 16 h–20 h | <0.001# | ||
| 20 h–24 h | 20 h–24 h | <0.001# |
#,*P< 0.005
On evaluating the variation in pain relief among the subjects, it was observed that all patients reported of almost complete pain relief by 24 h of therapy which was more prominent in the combined group than the oral analgesics group. Furthermore, steep decrease in pain was observed in combined group compared to oral analgesics group at 16 h [Graph 1].

-
Graph 1: Line diagram representing the mean pain scores against time period among two groups.
DISCUSSION
Post-extraction pain has always been a nemesis for dental professionals and patients due to the considerable degree of inflammatory response involved. Oral administration of NSAIDs is among the common methods of handling post-extraction pain. However, they carry the risk of first-pass metabolism and significant amount of drug lost before it is systemically absorbed. There is also known to cause several adverse effects that are dose dependent.[5] Hence, the transdermal systems have been developed which can be an adjunct with oral and other traditional forms of pain management. Although topical NSAID patches have been reported to provide effective analgesia in post-extraction cases, according to a study report, 17.5% of patients using transdermal and topical NSAIDs reported systemic adverse effects, with one reported a case of gastrointestinal bleeding.[4]
The present study involved a split-mouth technique at which each patient acts as his/her own control, thus much of the intersubject variability is removed. Resulting in increased study power or a decrease in the number of participants required compared with a study in which patients receive only one intervention. As pain is a subjective phenomenon, by doing extraction on the same patient may eliminate this variability.[1]
Besides that, a window period of 1 week was given from the first extraction to the second extraction to allow complete elimination of the previous drug from the body before prescribing the patients with another set of medications along with the transdermal herbal patch. This affirms the effect of the transdermal herbal patch without any attribution of the previous medication.
The result in the present study demonstrated that pain relief provided by oral NSAIDs and transdermal herbal patch was more compared to oral NSAIDs alone. From the beginning until the 4th h of the 1st post-operative day, there was not a statistically significant difference in VAS score between herbal patches with oral NSAIDs to oral NSAIDs alone. However, in the 16th h, the VAS score for transdermal herbal patch showed significant difference thus appeared to show better pain control. This is probably because they had achieved a more constant therapeutically effective concentration by this time.
Similar to a study done by Kaur et al., they incorporate a herbal patch, PowerStrips at which patients using PowerStrips patch reported a statistically and clinically significant reduction in pain scores after 3 days postoperatively, similar to those achieved with transdermal diclofenac patches.[1] The mean VAS scores reduced considerably after 3-day application of PowerStrips patch in more than 90% of patients.
The present study utilized a transdermal herbal patch that consists of polymer matrix which controls the release of the herbal ingredients and an impermeable backing membrane that prevents the leaching of drug from the top. The herbal patch contains formulation of natural elements such as Boswellia, eucalyptus oil, methyl salicylate, menthol, and camphor.[6-8] None of the patients in the study reported back with complications such as gastritis or occurrence of localized erythematous rash or pruritus at the site of application of the transdermal patch. Thus, in terms of safety, the patch was well tolerated and did not cause any local or systemic adverse effects. The herbal patch was also convenient and easy to be applied by the patient alone. However, this study came with a limitation at which it was only done on a controlled and sterilized environment. All the subjects for the study had a healthy periodontal status with none of their teeth being extensive decayed or periapically involved. Thus, the efficacy in pain management might be impaired if transdermal herbal patch being used in an infected extraction case.
CONCLUSION
Transdermal herbal patch seems to be a promising analgesic modality for the management of mild-to-moderate pain following dental extractions. It is evident from the results that transdermal herbal patches have a potent analgesic action with virtually no systemic adverse effects. This novel technology may have a role to play in the management of post-traumatic pain. However, as the present study is the first of its kind to evaluate its effectiveness, longer clinical trials with a larger sample size need to be conducted among diverse populations before the real scope of this technology can be clearly defined.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Efficacy of power strips as an alternate pain relief method in dental extractions: A clinical trial. Int J Community Med Public Health. 2016;3:1383-7.
- [CrossRef] [Google Scholar]
- Topical menthol increases cutaneous blood flow. Microvasc Res. 2016;107:39-45.
- [CrossRef] [PubMed] [Google Scholar]
- Central mechanisms of menthol-induced analgesia. J Pharmacol Exp Ther. 2012;343:661-72.
- [CrossRef] [PubMed] [Google Scholar]
- Transdermal and oral diclofenac in orthodontic premolar extractions. Contemp Clin Dent. 2010;1:158-63.
- [CrossRef] [PubMed] [Google Scholar]
- Relyon Pas Plus Transdermal Patch Pain Relief. 2010. Available from: https://www.indiamart.com/proddetail/pain-reliever-patch-19911128662.html [Last accessed on 2019 Oct 19]
- [Google Scholar]
- Comparison of transdermal diclofenac patch with intramuscular diclofenac injection as an analgesic modality following surgical extraction of impacted mandibular third molars: A cross over efficacy trail. Int J Sci Study. 2016;4:117-23.
- [Google Scholar]






