Translate this page into:
Soft-tissue paradigm: A review

*Corresponding author: Vivek Kumar Thakur, Department of Orthodontics and Dentofacial Orthopedics, Army Dental Centre (R and R), Army Hospital (R and R), Delhi, India. thakurvivek13@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Thakur VK, Chaudhary DC, Jayan B, Jain V, Mathur P. Soft-tissue paradigm: A review. J Global Oral Health 2023;6:107-14.
Abstract
Facial esthetics and balanced facial proportions are the expectations of the orthodontic patient. Promising and achieving the desired facial esthetic outcome, with functional harmony are the major orthodontic challenges. A detailed study of facial hard and soft-tissue structures is required for an orthodontist to evaluate, diagnose, and treat the chief complaints of an individual orthodontic patient. Orthodontic treatment has evolved from the angles paradigm to the soft-tissue paradigm. Evaluation in terms of facial esthetics requires a thorough understanding of the concept of the soft-tissue paradigm. This review article summarizes existing major facial esthetic parameters comprehensively and will also act as a guide for the detailed scientific evaluation of soft-tissue proportions in achieving treatment goals in orthodontics and dentofacial orthopedics.
Keywords
Soft-tissue paradigm
Facial proportions
Facial esthetics
INTRODUCTION
The face is the mirror of the mind and the soft-tissue drape which covers the facial skeleton and dentition greatly influences the physical and esthetic appearance of an individual. Orthodontists need to make every effort to develop a harmonious balance that will produce the most esthetic appearance and pleasant smile possible for each patient being treated. Angle believed that the diagnosis and treatment planning should focus on skeletal and dental components and the soft-tissue relationships were the consequence.[1] The functional matrix theory by Moss clarified the controversy of form following function versus function following form. These concepts changed as the experience of orthodontists over the decades found that hard tissue dogma has failed to achieve desired esthetic goals.[2]
Orthodontic, orthopedic, and orthognathic procedures bring about changes in the tooth position, skeletal relation, and soft-tissue profile. Orthodontic diagnosis, treatment planning, and prognosis are intimately related to the orthodontist’s concepts of dentofacial esthetics with due consideration given to muscular balance and harmony of the dental arches. Ackerman et al., summarized the contemporary conceptual changes that give primary emphasis to soft-tissue analysis of the face along with the importance of functional occlusion as a soft-tissue paradigm.[3] This review article aims to comprehensively summarize and highlight various facial soft-tissue esthetic parameters under one umbrella for enhanced utility and ready referencing.
LITERATURE REVIEW
The importance of facial esthetics is known to everyone and the scientific basis of the evolution of the concept of facial esthetics has a long and ancient history. The earliest reference can be traced back to ancient Egyptian culture, the fascinating concept of facial esthetics and its dynamism is built over the strong foundation of landmark efforts carried out by Da Vinci et al., experimental studies of Duchene, and many more [Figure 1].[4]
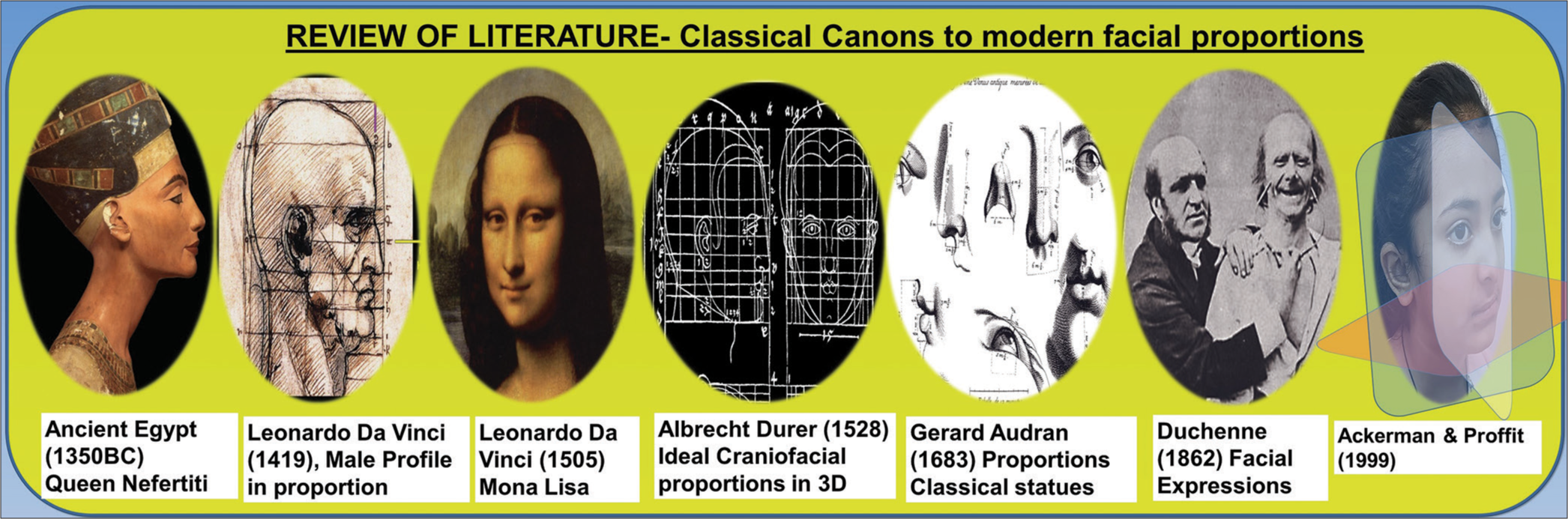
- Review of the literature.
Current orthodontic literature provides sufficient armamentarium to assess facial esthetics and soft-tissue balance. Clinical evaluation techniques form the core of this evaluation along with adjunctive techniques such as photographic analysis,[5,6] wiggle diagram[7] (simplified the practical problem of appraising faces for orthodontic needs by Hellman 1939), diagnostic facial triangle[8] (given special attention to esthetics by Tweed 1944), Correlation between hard-and soft-tissue changes along with the studies on lip posture, lip length, lower facial third characteristics,[9,10] soft-tissue analysis,[11,12] age changes in orthodontics,[13] correlation of malocclusion with perception of personality and other traits,[14] use of eye tracking software to evaluate facial esthetic components,[15,16] evaluation of attractiveness of smiling faces,[17] and facial esthetics and plastic surgery trends.[18] From historical background to the eminent modern craniofacial scientists and researchers such as Naini et al., and Ackerman et al., provided substantial literature on the subject of esthetic facial proportion helping in contemporary understanding of facial beauty.[3,19]
A CONCEPT OF FACIAL ESTHETICS
Perception and esthetic attitude are philosophically expressed by the famous quote “Beauty is in the eye of the beholder” by Hungerford[20] (1878). While the study of the face as the “esthetic stimulus” is still important, of equal significance now is the nature of the “esthetic response.” Wuerpel in the year 1936 mentioned the importance of the study of face and shortcomings in the Angle’s understanding of the concept of ideal occlusion and esthetics.[21] Therefore, he must have multiple objective methods for evaluating the face at his disposal.
SUBJECTIVE PERCEPTION OF FACIAL ESTHETICS
A person’s subjective view of someone’s facial characteristics attractiveness and appeal is referred to as their subjective sense of facial esthetics. Facial symmetry, dimensions, skin tone, facial features (such as the eyes, nose, and lips), and overall face harmony are just a few examples of the many components that make up facial esthetics. These characteristics may affect how others view a person’s appearance and attractiveness. It is crucial to remember that beauty is a relative concept that can be influenced by cultural, social, and individual aspects.[19] The definition of beauty in society is continuously changing, and what is seen as attractive may alter over time.[22] However, if a patient with a facial deformity is viewed, practically everyone will concur that the face is malformed and not physically attractive, proving that when it comes to deformities, beauty is no longer in the eye of the beholder. This article attempts to summarize available evidence-based established norms. The facial esthetics can be evaluated under the following broad subheads.
FACIAL PROPORTIONS
Proportions and symmetry are important components of esthetics. The rule of horizontal fifths and vertical thirds is well known. Ricketts[23] (1982) extrapolated the concept of the golden proportion (phi) and Fibonacci series into orthodontics. Facial index (FI) is one such measure for evaluating facial proportion using the following formula: FI = Facial length/Bizygomatic width × 100 (mesoprosopic = 84–88).
FIVE FACIAL PROMINENCES
According to Aufricht (1958), the forehead, nose, lips, chin, and submental-cervical region are the important component of facial esthetics and their evaluation is as important as their relative interrelationship.[24]
Forehead: In profile evaluation, it is described as protrusive, flat, posteriorly inclined, and anteriorly inclined. According to Farkas[25] (1994), the normal adult has a mild posterior inclination; in males, it is 10 ± 4° and in females 6 ± 5°. At times the prominent supraorbital rim or forehead, frontal bossing, may be found associated with many syndromic conditions such as Crouzon syndrome, Pfeiffer syndrome, Russell–Silver syndrome, Rubinstein–Taybi syndrome, Hurler syndrome, and acromegaly, altering this normal inclination and providing us with an opportunity to diagnose the underlying condition for greater patient benefit. Thus, knowledge of normal and abnormal is equally important for an orthodontist.
Nose: This is the most prominent part of the facial profile. Parts of the nose to be evaluated are the radix, dorsum, sidewall, tip lobule, ala, soft triangle, and columella.
The nose is classified in many ways such as long, short, high at the tip, low at the tip[26] or as aquiline nose (also known as Roman nose seen in many native American tribes), celestial nose (upturn nose most common in Europe), Greek nose (narrow nostril and pointed tip), nubian nose (long with wide base seen in Africans), and small nose (short nose).
The nasal index (NI: NI by Farkas and Munro is evaluated as nasal interalar width/nose height (N’-Sn) × 100. Based on NI noses can be platyrrhine, mesorrhine (NI 65 ± 5), and leptorrhine[27] [Figure 2].
Growth of nasal bone completed by the age of 10–12 years followed by the considerable growth of nasal cartilage and soft tissue during adolescence and subsequent age changes.[28]
-
Nasolabial angle: Different authors and researchers have given different norms for nasolabial angle depending on the population under study. Some comparative measures usually used in orthodontic diagnosis are:
According to Burstone et al.,[29] (1980) it is formed by the upper lip and base of the nose with an average value of 102 ± 4°.
Scheideman et al.,[30] (1980) divided it as upper nasolabial angle (UNLA)= 25° and lower nasolabial angle (LNLA)= 85°.
According to Fitzgerald et al.,[31] (1992) Nasolabial angle is 114 ± 10°. The nasolabial angle is further divided into UNLA and LNLA. The UNLA is measured from the FH plane to the lower border of the nose (18 ± 7) and LNLA from the FH plane to the upper lip (98 ± 5°).
Burstone provided a reasonable measure of nasal esthetics, though differentiation between UNLA and LNLA adds to the distinct contribution to this angle by the nose and lip.[29]
Nose prominence (1983): Nasal prominence (NP) is usually evaluated with Holdaways’ analysis[10] NP <14 mm is considered small, and more than 24 mm is considered large. This indicates nose type and guides in the relative evaluation of projection of other facial prominences.
Arnett and Bergman analysis[12] (1993): Nasal base lip contour and nasal projection are considered.

- Nasal index.
Lips: Lips are one of the most important components of facial static and functional evaluation. Parts of the lip include philtrum, philtral ridges/columns, cupids bow, white roll, upper lip vermilion, upper lip tubercle, vermilion border, lower lip vermilion, oral commissures, nasolabial groove, and mentolabial groove. Sabri (2005) gives eight valuable smile evaluation tools namely, lip line, smile arc, upper lip curvature, lateral negative spaces, smile symmetry, occlusal frontal plane, dental component, and gingival component.[32]
Clinical evaluation of lips should include the following algorithm of LAMPP (lip Lines, lip Activity, lip Morphology, lip Posture, lip Prominence).
Lip lines – vertical positions of the upper and lower lips to the anterior dentition. About 2–4 mm of maxillary incisor (MI) exposure is considered normal at rest. (i) High upper lip line or gummy smile, (ii) low upper lip line or no tooth smile, (iii) high lower lip line as in Class II Division 2 cases, and (iv) low lower lip line when there is increased lower anterior facial height (LAFH).
Lip activity – dynamic lip evaluation, that is lip function is dependent on the muscular tone of the lips. Based on this lip activity can be, overactive or hypertonic, underactive or hypotonic.
Lip morphology – includes various parameters. (i) The upper lip length, measured from subnasale to stomion superius. The norms (Burstone[9]) for adult males are 22 ± 2 mm and females 20 ± 2 mm, which matches most populations. (ii) The lower lip length measured from stomion to sublabiale, the norms for adult males are 20 ± 2 mm and females 18 ± 2 mm, (iii) lip thickness as per ethnic variation can be thick lips, thick flaccid lips, or thin lips, (iv) the lip contour that is lip curl can be excessive lip curl or reduced lip curl, and (v) the lip curvature was evaluated with the comparison of philtrum height and commissure height. There can be normal curvature or reverse lip (gull lip) curvature mostly seen in cases with vertical maxillary excess [Figure 3].
Lip posture – evaluation of lip competency (competent lips, incompetent lips, and potential lip competence).
Lip prominence – is described by a few terms such as lip projection, protrusive lips, and retrusive lips.
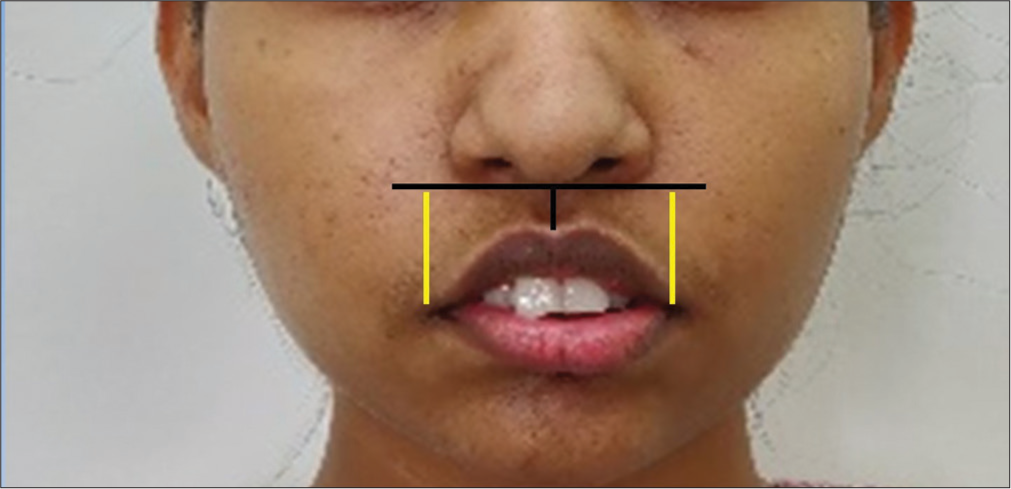
- Gull lip (Reverse lip curvature).
Chin: Chin projection in frontal and profile view is another important parameter in clinical examination. Mentolabial fold greatly influences chin appearance, which in turn is associated with LAFH. The association of the chin with growth rotation and growth pattern has numerous studies in the literature.[33,34] The relative chin position with nose and lip prominence is the area of interest in facial esthetic evaluation.
The practical query [Figure 4] now is, how to choose among the various esthetic profile lines as a norm for an individual with an aberrant soft-tissue profile [Figure 4(?)] as each of these profile analyses is based on their specifically defined landmarks. When the particular landmark, for example, nasal tip (Prn) is aberrant in an individual then Ricketts E-line cannot be taken as a norm for that individual and we need to choose another profile line to set as soft-tissue profile norm. Z-line or Riedel plane might provide a better guideline if the nasal tip is aberrant [Figure 4].
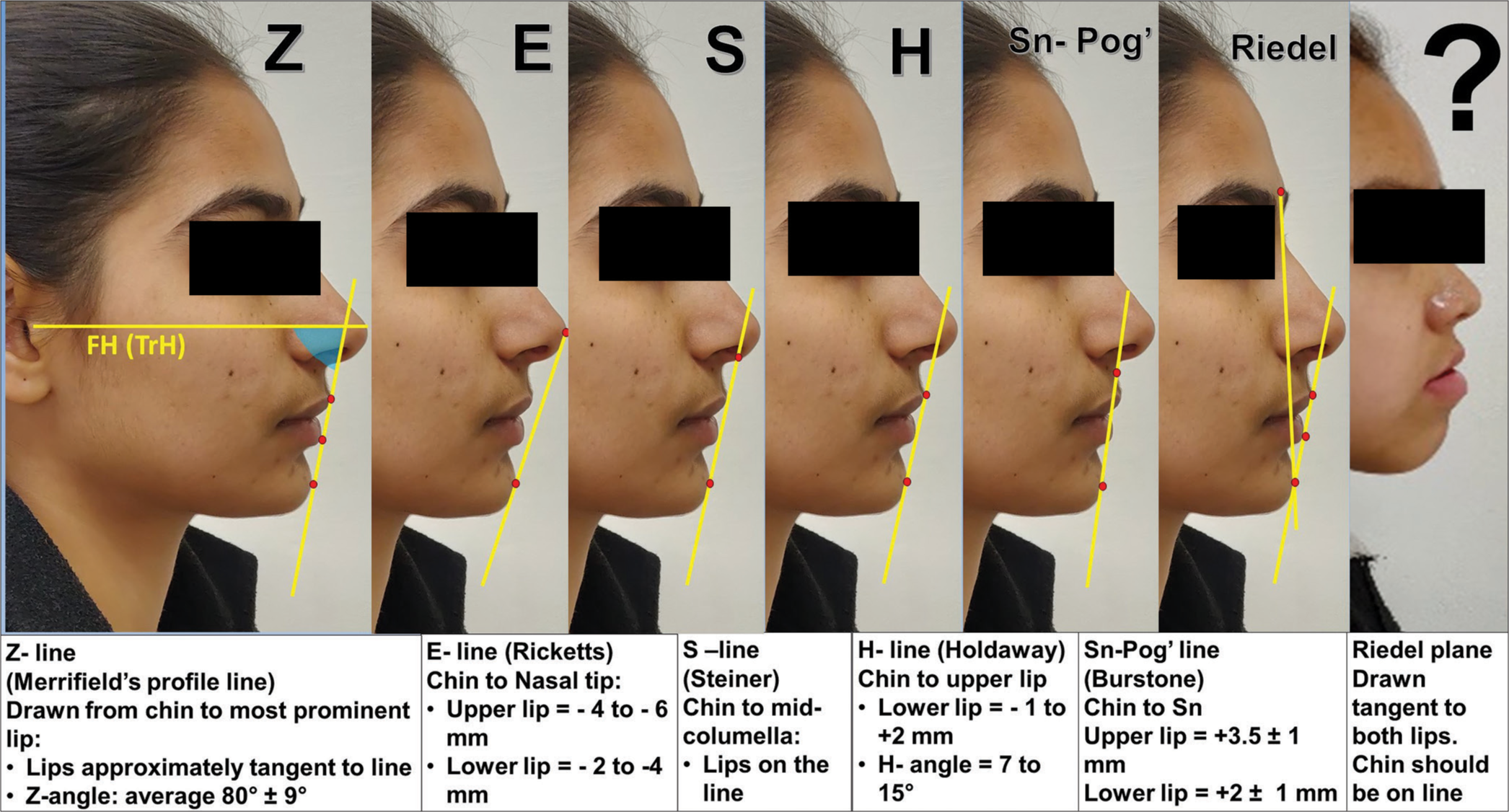
- Profile analysis. FH: Frankfort horizontal plane, TrH: True horizontal plane. (?) An aberrant facial profile, an aberrant soft-tissue profile as mentioned in the text is shown as Figure 4 (?).
Submental cervical region – The jawline, hyoid bone position (muscle-determined suspended bone position), fat deposition, and neck musculature are major determinants of the youthful esthetic or unesthetic appearance of the face. For example, in cases with mandibular prognathism, the surgical mandibular setback will lead to the bunching of submental soft tissues and may lead to an unesthetic overall outcome if not taken into consideration during treatment planning.
PLANNED INCISOR POSITION (PIP)
The end treatment intended for MI position is known as the PIP.[35] It involves determining the ideal position of the upper and lower incisors in the dental arch. The goal of PIP is to achieve optimal esthetics, function, and stability for the patient. Orthodontic treatment planning takes into consideration various factors and guidelines to achieve the best possible outcome:
Facial esthetics: The position of the incisors plays a crucial role in overall facial esthetics. Evidence suggests that certain established esthetic norms are generally considered desirable. These include factors such as lip support, smile arc, and the relationship between the incisors and other facial features. The use of standardized facial analyses, such as the Steiner analysis, Ricketts’ analysis, and Arnett analysis, can help guide orthodontists in planning the incisor position.[12]
Soft-tissue profile: Particularly the relationship between the lips and the incisors, is an important consideration in determining the incisor position. The position of the incisors can influence the lip support and balance, which can impact the overall esthetics of the face. Guidelines, such as the Holdaway analysis or the Merrifield analysis, provide measurements and ratios that can aid in determining the ideal incisor position with the soft tissues.[11]
Functional considerations: The position of the incisors also affects occlusal function, including factors such as incisal guidance, overjet, and overbite. These functional considerations play an important role in determining the incisor position to achieve functional occlusion and stable long-term outcomes. Guidelines, such as the Andrews’ six elements of Orofacial Harmony™ provide insights into static and functional considerations when planning incisor position.[36]
Individualized treatment: Each patient’s case is unique, and orthodontic treatment planning should consider individual factors such as facial and dental proportions, skeletal discrepancies, and specific malocclusions. Evidence-based orthodontics emphasizes the importance of individualized treatment planning, taking into account patient-specific factors to achieve optimal results.
In summary, the goal of orthodontic treatment is to achieve a stable and esthetic lip–incisor relationship. PIP is determined and affected by seven interrelated factors that are (i) upper lip length, (ii) upper lip activity, (iii) vertical position of MIs and premaxilla (PM), (iv) sagittal positioning of MI and PM, (v) inclination of MI and PM, (vi) crown height, and (vii) gingival margins.
FUNCTIONAL CONSIDERATIONS IN FACIAL ESTHETICS
In orthodontics, functional aspects of face symmetry are very important. Orthodontic treatment seeks to produce both harmonious face esthetics and balanced functional occlusion. The following are some crucial functional facial esthetic orthodontic considerations.[37]
Dental occlusion: A mutually protected occlusion is one of the functional goals to achieve to facilitate effective chewing, reduce tooth wear, and improve facial harmony.
Lip support: A balanced and esthetically pleasant smile depends on the relationship between the teeth and lips during rest and function. The activity and tonicity of the orbicularis oris, zygomaticus major, levator anguli oris, depressor anguli oris, and risorius muscles play an important role in a dynamic smile during function.
Considerations for soft tissue: The lips, cheeks, chin, submental tissues, tongue, and soft palate are among the soft tissues that are considered during esthetic evaluation. Improved face esthetics can result from proper jaw and tooth alignment, which has a good effect on the balance and support of the soft tissues during function.
Smile arc: For a smile to appear pleasant and natural, a good smile arc must be achieved. By straightening the teeth and taking into consideration their proportion, position, and shape, orthodontic therapy seeks to create a harmonious grin arc.
Health of the temporomandibular joint (TMJ): To maintain optimal function and reduce the risk of TMJ diseases, orthodontic treatment takes the link between the teeth, jaws, and TMJ into account.
AIRWAY EVALUATION
The evolution and development of maxillofacial structures are to sustain the basic function of breathing and maintenance of the airway. In orthodontics, airway evaluation has gained significant attention in recent years due to its importance in assessing the relationship between orthodontic treatment and the patient’s overall airway health. In borderline cases with orthodontic/orthognathic procedures, compromise on facial esthetics is acceptable over airway compromise. Airway-centric orthodontics is the path to achieving long-term stability in treated orthodontic cases.[38,39] Here are some key points regarding airway evaluation in orthodontics:
Importance of airway evaluation: The airway plays a crucial role in overall health and well-being. Orthodontic treatment has the potential to impact the airway, either positively or negatively. Therefore, evaluating the airway is important to identify any potential issues that may arise during or after orthodontic treatment.
Several signs and symptoms may indicate an airway problem, including mouth breathing, snoring, sleep apnea, daytime drowsiness, chronic allergies, and narrow or high-arched palate. These indicators may prompt the need for a comprehensive airway evaluation.
Orthodontic examination: The functional analysis highly recommends clinical examination of tongue function, posture, evaluation of soft palate, and breathing pattern of each orthodontic patient. Airway analysis must be carried out before concluding the diagnostic summary and treatment plan of an orthodontic case.
Diagnostic tools: STOP-Bang questionnaire, modified Mallampati score, Epworth sleepiness Scale, Friedman tongue position, Pediatric Sleep Questionnaire, Epworth Sleepiness Scale for Children and Adolescents, Brodsky tonsil grades, Friedman tonsil grading system, body mass index, lateral cephalogram analysis, cone-beam computed tomography, and magnetic resonance imaging. However, polysomnography remains the gold standard in diagnostic investigation.
Interdisciplinary approach: In complex cases, orthodontists may collaborate with other health-care professionals; such as otorhinolaryngologists, sleep medicine specialists, oral and maxillofacial surgeons, and plastic and reconstructive surgeons. This interdisciplinary approach ensures a comprehensive evaluation of the airway and facilitates appropriate treatment planning.
CLINICAL IMPLICATIONS
Facial soft-tissue balance holds the key to the esthetic outlook of the patient and the cumulative knowledge of orthodontic standards, and racial and regional variability will play a decisive role in planning the outcome. One should not always be obsessed with the numerical values in reaching the desired objectives. Hence, the following clinical implications should be kept in mind during the clinical evaluation and treatment planning of every orthodontic patient:
Facial profile changes following orthopedic, orthodontic, or orthognathic treatment
Whether to extract or not to extract in borderline cases
Diagnosis and treatment planning as per facial types, growth patterns, and airway
Facial profile changes after therapeutic extraction protocol, genioplasty, and orthognathic surgery cases
Age changes in facial soft-tissue profile need due consideration while planning and treating a case
CONCLUSION
The logical development of visual treatment objectives and providing the most realistic treatment outcome is the key. Achieving optimal facial harmony and understanding the limitation of soft-tissue drapes over dental and skeletal structures are of prime importance. This review article will help as a guide for the detailed scientific evaluation of soft-tissue proportions in achieving treatment goals in orthodontics and dentofacial orthopedics.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Malocclusion of the teeth (7th ed). Philadelphia, PA: S.S. White Dental MFG. Co.; 1907.
- [Google Scholar]
- The functional matrix In: Kraus B, Reidel R, eds. Vistas in orthodontics. Philadelphia, PA: Lea & Febiger; 1962. p. :85-98.
- [Google Scholar]
- The emerging soft tissue paradigm in orthodontic diagnosis and treatment planning. Clin Orthod Res. 1999;2:49-52.
- [CrossRef] [PubMed] [Google Scholar]
- Leonardo da Vinci: The marvellous works of nature and man Oxford: Oxford University Press; 2006.
- [Google Scholar]
- Roentgenostatics: A practical evaluation of the x-ray headplate. Am J Orthod. 1961;47:561-85.
- [CrossRef] [Google Scholar]
- Some facial features and their orthodontic implication. Am J Orthod Oral Surg. 1939;25:927-51.
- [CrossRef] [Google Scholar]
- Indications for extraction of teeth in orthodontic procedure. Am J Orthod. 1944;42:22-45.
- [CrossRef] [Google Scholar]
- Lip posture and its significance in treatment planning. Am J Orthod. 1967;53:262-84.
- [CrossRef] [PubMed] [Google Scholar]
- A longitudinal study of soft tissue facial structures and their profile characteristics, defined in relation to underlying skeletal structures. Am J Orthod. 1959;45:481-507.
- [CrossRef] [Google Scholar]
- A soft-tissue cephalometric analysis and its use in orthodontic treatment planning. Part I. Am J Orthod. 1983;84:1-28.
- [CrossRef] [PubMed] [Google Scholar]
- Facial keys to orthodontic diagnosis and treatment planning: Part I. Am J Orthod Dentofac Orthop. 1993;103:299-312.
- [CrossRef] [PubMed] [Google Scholar]
- Linear changes of the maxillary and mandibular lips. Am J Orthod Dentofacial Orthop. 1988;94:405-10.
- [CrossRef] [PubMed] [Google Scholar]
- Malocclusions and perceptions of attractiveness, intelligence, and personality, and behavioral intentions. Am J Orthod Dentofacial Orthop. 2011;140:669-79.
- [CrossRef] [PubMed] [Google Scholar]
- The contribution of dental attractiveness and female facial attractiveness to smile esthetics evaluated by eye tracking. Am J Orthod Dentofacial Orthop. 2015;147:472-82.
- [CrossRef] [PubMed] [Google Scholar]
- Objective assessment of the contribution of dental esthetics and facial attractiveness in men via eye tracking. Am J Orthod Dentofacial Orthop. 2018;153:523-33.
- [CrossRef] [PubMed] [Google Scholar]
- Contribution of facial components to the attractiveness of the smiling face in male and female patients: A cross-sectional correlation study. Am J Orthod Dentofacial Orthop. 2020;157:98-104.
- [CrossRef] [PubMed] [Google Scholar]
- Evolution and trends of facial plastic surgery and facial aesthetic procedures in India: From awakening to revival. Aesthet Surg J Open Forum. 2023;5:ojad022.
- [CrossRef] [PubMed] [Google Scholar]
- The enigma of facial beauty: Esthetics, proportions, deformity, and controversy. Am J Orthod Dentofac Orthop. 2006;130:277-82.
- [CrossRef] [PubMed] [Google Scholar]
- What makes a face attractive and why: The role of averageness in defining facial beauty In: Rhodes G, Zebrowitz LA, eds. Facial attractiveness: Evolutionary, cognitive, and social perspectives. Advances in visual cognition. Vol 1. London: Ablex Publishing; 2002.
- [Google Scholar]
- The biologic significance of the divine proportion and Fibonacci series. Am J Orthod. 1982;81:351-70.
- [CrossRef] [PubMed] [Google Scholar]
- Combined plastic surgery of the nose and chin; résumé of twenty-seven years' experience. Am J Surg. 1958;95:231-6.
- [CrossRef] [PubMed] [Google Scholar]
- Elements of morphology: Standard terminology for the nose and philtrum. Am J Med Genet A. 2009;149A:61-76.
- [CrossRef] [PubMed] [Google Scholar]
- Anthropometric facial proportions in medicine United States: Springfield: Charles C Thomas; 1987.
- [Google Scholar]
- Rhinosurgery in children: Developmental and surgical aspects of the growing nose. Laryngorhinootologie. 2010;89(Suppl 1):S46-71.
- [Google Scholar]
- Cephalometric analysis of dentofacial normals. Am J Orthod. 1980;78:404-20.
- [CrossRef] [PubMed] [Google Scholar]
- An evaluation of the nasolabial angle and the relative inclinations of the nose and upper lip. Am J Orthod Dentofacial Orthop. 1992;102:328-34.
- [CrossRef] [PubMed] [Google Scholar]
- Variations in the growth pattern of the human mandible: Longitudinal radiographic study by the implant method. J Dent Res. 1963;42:400-11.
- [CrossRef] [PubMed] [Google Scholar]
- Effective condylar growth and chin position changes in activator treatment: A cephalometric roentgenographic study. Angle Orthod. 2001;71:4-11.
- [Google Scholar]
- Obstructive sleep apnea and orthodontics: An American Association of orthodontists white paper. Am J Orthod Dentofacial Orthop. 2019;156:13-28.e1.
- [CrossRef] [PubMed] [Google Scholar]






